- Record: found
- Abstract: found
- Article: found
Post-transfusion severe headache in a patient with thalassemia with superficial siderosis of the central nervous system: a case report and literature review
Read this article at
Abstract
Background
Patients with severe thalassemia may experience adverse effects from transfusion such as fever, rash, and iron overload after long-term transfusion therapy. Severe headaches as a side effect of blood transfusion in patients with thalassemia are not commonly observed, especially when combined with superficial siderosis of the central nervous system, which is easily misdiagnosed and requires excessive examination and treatment.
Case Presentation
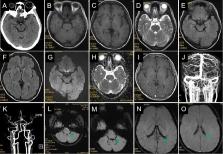
A 31-year-old woman was admitted with severe headache and vomiting over 3 days following blood transfusion. She was diagnosed with intermediate α-thalassemia at 2 years of age and had a history of irregular blood transfusions. Physical examination revealed horizontal nystagmus with no other abnormal neurological signs. Magnetic resonance (MR) imaging, MR venography, MR arteriography, and cerebrospinal fluid analysis were normal. However, susceptibility-weighted imaging showed abnormal signals in the bilateral and fourth ventricles. Initial antibiotics, antivirals, decompression of intracranial pressure, iron chelation, and symptomatic treatments were administered; subsequently, small intermittent blood transfusions were cautiously administered for severe anemia. The patient’s headache was gradually relieved, and she was discharged on day 9. At the 5-month follow-up, the patient’s headache recurred following another transfusion.
Conclusions
Severe post-transfusion headache in patients with thalassemia has not been fully recognized and is easily misdiagnosed, leading to excessive examination and treatment. Understanding the clinical features of transfusion-related headaches can help identify this complication, but the exact pathophysiological mechanism requires further research.
Related collections
Most cited references40
- Record: found
- Abstract: found
- Article: not found
Global epidemiology of haemoglobin disorders and derived service indicators.
- Record: found
- Abstract: found
- Article: not found
The pathology of superficial siderosis of the central nervous system.
- Record: found
- Abstract: found
- Article: not found