- Record: found
- Abstract: found
- Article: not found
Clinical Significance of On-Treatment Triglyceride Level in Patients Treated by Percutaneous Coronary Intervention for Non-ST-Segment Elevation Acute Coronary Syndrome
Read this article at
Abstract
Background/Aims
The use of statins in patients with acute coronary syndrome (ACS) has increased, and reduced levels of low-density lipoprotein cholesterol (LDL-C) lead to lower coronary event rates. We studied the effect of lipid levels during statin treatment on prognosis in patients with ACS and percutaneous coronary intervention (PCI).
Methods
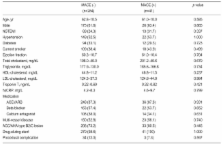
Between January 2005 and May 2007, 325 ACS patients who underwent PCI and received statins were evaluated. We measured serum lipid levels at baseline and 4 weeks. The relationships between on-treatment levels of triglyceride (TG) and LDL-C and one-year major adverse cardiac events (MACE) were assessed.
Results
At 4 weeks, the mean LDL-C level was 72.5±23.8 mg/dL and the mean TG was 123.2±62.8 mg/dL. MACE occurred in 41 cases (12.6%). Baseline serum lipid levels were similar between the patients with and those without MACE. However, the patients with MACE showed significantly higher TG level at 4 weeks (149.6±81.4 vs. 119.3±58.9 mg/dL, p=0.026) than those without. High on-treatment TG level (≥150 mg/dL) were associated with increased adverse events compared to lower TG level in a univariate analysis (hazard ratio [HR], 3.3; p<0.001). In a multivariate analysis, high 4-week TG level after statin treatment was an independent predictor for MACE (HR, 4.01; 95% confidence interval, 1.85 to 9.06; p=0.001), however, baseline TG and LDL-C levels were not.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S)
- Record: found
- Abstract: found
- Article: not found
Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies.
- Record: found
- Abstract: found
- Article: not found
