- Record: found
- Abstract: found
- Article: found
Predictors of Out of Hospital Cardiac Arrest Outcomes in Pre-Hospital Settings; a Retrospective Cross-sectional Study
Read this article at
Abstract
Introduction:
Different potential factors can affect the outcomes of Out of Hospital Cardiac Arrest (OHCA). The present study aimed to identify important factors contributing to the Return of Spontaneous Circulation (ROSC) and Survival to Hospital Discharge (SHD) in these patients.
Methods:
This cross-sectional study was conducted on all the OHCA patients who underwent Cardiopulmonary Resuscitation (CPR) in emergency medical service (EMS) of Hamedan province during 2016-2017. All the relevant data were retrieved from three sources, according to Utstein’s style. In addition, univariate and multivariate logistic regressions were employed to identify predictive factors of ROSC and SHD using SPSS software, version 20.
Results:
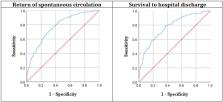
Among the 3214 eligible patients whose data were collected, most OHCA patients were female (59.7%) with the mean age of 58 years. Moreover, the majority of OHCAs (77.8%) occurred at home during 8pm-8am (65.1%) and about 26.3% of OHCAs were witnessed, with only 5.1% bystander-initiated CPR. Furthermore, the median ambulance response time and CPR duration were 6.0 and 20 minutes, respectively. Overall, ROSC and SHD success rates were 8.3 and 4.1%, respectively. Bystander CPR was found to be the most effective predicting factor for the success rate of ROSC (AOR=3.26, P<0.001) and SHD (AOR=3.04, P<0.001) after adjusting for the Utstein variables including the patients’ age, gender, cardiac disease history, arrest time, CPR duration, response time, being witnessed, bystander CPR, and endotracheal intubation (ETI).
Conclusion:
The overall success rates of ROSC and SHD were 8.3% and 4.1%, respectively. The age, ambulance response time, CPR duration, and cardiac disease history were negatively associated with the outcomes of ROSC and SHD, while being witnessed, bystander CPR, ETI, and initial shockable rhythm were positively related to both of the above-mentioned outcomes.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies?

- Record: found
- Abstract: found
- Article: not found