- Record: found
- Abstract: found
- Article: found
The Impact of Hypotensive Epidural Anesthesia on Distal and Proximal Tissue Perfusion in Patients Undergoing Total Hip Arthroplasty
Read this article at
Abstract
Little data exists to detail the effect of hypotensive epidural anesthesia on differential tissue oxygenation changes above and below the level of neuraxial blockade. This study was designed to investigate tissue oxygenation in a clinical setting, using non-invasive near-infrared spectroscopy.
Methods
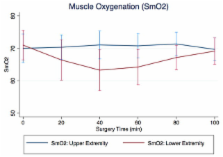
Patients aged 18 to 85 years scheduled to undergo primary total hip arthroplasty were enrolled. Muscle oxygenation saturation was measured above and below the level of neuraxial blockade (deltoid and vastus lateralis muscles). Other continuously recorded parameters included cardiac output, stroke volume, heart rate, invasive mean arterial blood pressure and arterial oxygen saturation. Recordings of muscle oxygenation were compared over time separately for upper and lower extremity.
Results
10 patients were enrolled. We found an intermittent and significant unadjusted decline of mean muscle oxygenation saturation in the vastus lateralis muscle during first part of the surgery (nadir 2 nd quintile: 71.0% vs. 63.3%, p<0.0001). This decline was followed by a return to baseline towards the end of the surgery (71.0% vs. 69.1%, p=0.3429). Mean muscle oxygenation saturation did not change for the same period of time in the deltoid muscle. When adjusting for covariates, the changes in muscle tissue oxygenation remained significant.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis.
- Record: found
- Abstract: found
- Article: not found
Randomized trial of hypotensive epidural anesthesia in older adults.
- Record: found
- Abstract: found
- Article: not found