- Record: found
- Abstract: found
- Article: found
Risk of Suicide After Cancer Diagnosis in England
Key Points
Question
What is the risk of suicide after cancer diagnosis in England, and which subgroups of patients are most at risk?
Findings
In this population-based study of 4 722 099 adult patients with cancer, a 20% increased risk of suicide compared with the general population was noted, corresponding to 0.19 excess deaths per 10 000 person-years. Patients with mesothelioma, pancreatic, esophageal, and lung cancer had the highest risk.
Meaning
The first 6 months after diagnosis of cancer has been shown to be a critical period, identifying the time during which cancer care pathways should pay particular attention to the psychological health needs of the patients; as suicide is hard to predict, all patients should receive improved psychological support.
Abstract
Importance
A diagnosis of cancer carries a substantial risk of psychological distress. There has not yet been a national population-based study in England of the risk of suicide after cancer diagnosis.
Objectives
To quantify suicide risk in patients with cancers in England and identify risk factors that may assist in needs-based psychological assessment.
Design, Setting, and Participants
Population-based study using data from the National Cancer Registration and Analysis Service in England linked to death certification data of 4 722 099 individuals (22 million person-years at risk). Patients (aged 18-99 years) with cancer diagnosed from January 1, 1995, to December 31, 2015, with follow-up until August 31, 2017, were included.
Main Outcomes and Measures
All deaths in patients that received a verdict of suicide or an open verdict at the inquest. Standardized mortality ratios (SMRs) and absolute excess risks (AERs) were calculated.
Results
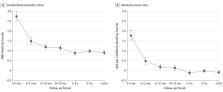
Of the 4 722 099 patients with cancer, 50.3% were men and 49.7% were women. A total of 3 509 392 patients in the cohort (74.3%) were aged 60 years or older when the diagnosis was made. A total of 2491 patients (1719 men and 772 women) with cancer died by suicide, representing 0.08% of all deaths during the follow-up period. The overall SMR for suicide was 1.20 (95% CI, 1.16-1.25) and the AER per 10 000 person-years was 0.19 (95% CI, 0.15-0.23). The risk was highest among patients with mesothelioma, with a 4.51-fold risk corresponding to 4.20 extra deaths per 10 000 person-years. This risk was followed by pancreatic (3.89-fold), esophageal (2.65-fold), lung (2.57-fold), and stomach (2.20-fold) cancer. Suicide risk was highest in the first 6 months following cancer diagnosis (SMR, 2.74; 95% CI, 2.52-2.98).
Conclusions and Relevance
Despite low absolute numbers, the elevated risk of suicide in patients with certain cancers is a concern, representing potentially preventable deaths. The increased risk in the first 6 months after diagnosis may indicate an unmet need for psychological support. The findings of this study suggest a need for improved psychological support for all patients with cancer, and attention to modifiable risk factors, such as pain, particularly in specific cancer groups.
Abstract
This population-based study examines the risk of suicide in patients in England after diagnosis of cancer, including cancer type and stage, time since diagnosis, and sociodemographic factors.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Suicide prevention strategies revisited: 10-year systematic review
- Record: found
- Abstract: found
- Article: not found
Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies.
- Record: found
- Abstract: not found
- Article: not found