- Record: found
- Abstract: found
- Article: found
Treatment of renal anemia: Erythropoiesis stimulating agents and beyond
Read this article at
Abstract
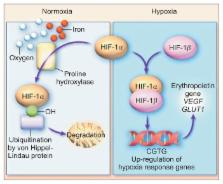
Anemia, complicating the course of chronic kidney disease, is a significant parameter, whether interpreted as subjective impairment or an objective prognostic marker. Renal anemia is predominantly due to relative erythropoietin (EPO) deficiency. EPO inhibits apoptosis of erythrocyte precursors. Studies using EPO substitution have shown that increasing hemoglobin (Hb) levels up to 10–11 g/dL is associated with clinical improvement. However, it has not been unequivocally proven that further intensification of erythropoiesis stimulating agent (ESA) therapy actually leads to a comprehensive benefit for the patient, especially as ESAs are potentially associated with increased cerebro-cardiovascular events. Recently, new developments offer interesting options not only via stimulating erythropoeisis but also by employing additional mechanisms. The inhibition of activin, a member of the transforming growth factor superfamily, has the potential to correct anemia by stimulating liberation of mature erythrocyte forms and also to mitigate disturbed mineral and bone metabolism as well. Hypoxia-inducible factor prolyl hydroxylase inhibitors also show pleiotropic effects, which are at the focus of present research and have the potential of reducing mortality. However, conventional ESAs offer an extensive body of safety evidence, against which the newer substances should be measured. Carbamylated EPO is devoid of Hb augmenting effects whilst exerting promising tissue protective properties. Additionally, the role of hepcidin antagonists is discussed. An innovative new hemodialysis blood tube system, reducing blood contact with air, conveys a totally different and innocuous option to improve renal anemia by reducing mechanical hemolysis.
Related collections
Most cited references107
- Record: found
- Abstract: found
- Article: not found
Correction of anemia with epoetin alfa in chronic kidney disease.
- Record: found
- Abstract: found
- Article: not found
A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease.
- Record: found
- Abstract: found
- Article: not found