- Record: found
- Abstract: found
- Article: not found
Safety and immunogenicity of a high-dose quadrivalent influenza vaccine administered concomitantly with a third dose of the mRNA-1273 SARS-CoV-2 vaccine in adults aged ≥65 years: a phase 2, randomised, open-label study
Read this article at
Abstract
Background
Concomitant seasonal influenza vaccination with a COVID-19 vaccine booster could help to minimise potential disruption to the seasonal influenza vaccination campaign and maximise protection against both diseases among individuals at risk of severe disease and hospitalisation. This study aimed to assess the safety and immunogenicity of concomitant administration of high-dose quadrivalent influenza vaccine (QIV-HD) and a mRNA-1273 vaccine booster dose in older adults.
Methods
This study is an ongoing, phase 2, multicentre, open-label, descriptive trial at six clinical research sites in the USA. We describe the interim results up to 21 days after vaccination (July–August, 2021). Community-dwelling adults aged 65 years and older, who were previously vaccinated with a two-dose primary schedule of the mRNA-1273 SARS-CoV-2 vaccine, were eligible for inclusion. The second dose of the primary mRNA-1273 vaccination series was required to have been received at least 5 months before enrolment in the study. Participants were randomly assigned (1:1:1) using a permuted block method stratified by site and by age group (<75 years vs ≥75 years), to receive concomitant administration of QIV-HD and mRNA-1273 vaccine, QIV-HD alone, or mRNA-1273 vaccine alone. Randomisation lists, generated by Sanofi Pasteur biostatistics platform, were provided to study investigators for study group allocation. Unsolicited adverse events occurring immediately, solicited local and systemic reactions up to day 8, and unsolicited adverse events, serious adverse events, adverse events of special interest, and medically attended adverse events up to day 22 were reported. Haemagglutination inhibition antibody responses to influenza A/H1N1, A/H3N2, B/Yamagata, and B/Victoria strains and SARS CoV-2 binding antibody responses (SARS-CoV-2 pre-spike IgG ELISA) were assessed at day 1 and day 22. All analyses were descriptive. The study is registered with ClinicalTrials.gov, NCT04969276.
Findings
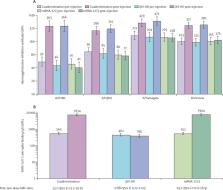
Between July 16 and Aug 31, 2021, 306 participants were enrolled and randomly assigned, of whom 296 received at least one vaccine dose (100 in the coadministration group, 92 in the QIV-HD, and 104 in the mRNA-1273 group). Reactogenicity profiles were similar between the coadministration and mRNA-1273 groups, with lower reactogenicity rates in the QIV-HD group (frequency of solicited injection site reactions 86·0% [95% CI 77·6–92·1], 91·3% [84·2–96·0], and 61·8% [50·9–71·9]; frequency of solicited systemic reactions 80·0%, [70·8–87·3], 83·7% [75·1–90·2], and 49·4% [38·7–60·2], respectively). Up to day 22, unsolicited adverse events were reported for 17·0% (95% CI 10·2–25·8) of participants in the coadministration group and 14·4% (8·3–22·7) of participants in the mRNA-1273 group, and tended to be reported at a slightly lower rate (10·9% [5·3–19·1]) in participants in the QIV-HD group. Seven participants each reported one medically attended adverse event (three in the coadministration group, one in the QIV-HD group, and three in the mRNA-1273 group). There were no serious adverse events, adverse events of special interest, or deaths. Haemagglutination inhibition antibody geometric mean titres increased from day 1 to day 22 to similar levels in the coadministration and QIV-HD groups, for each influenza strain (A/H1N1: 363 [95% CI 276–476] vs 366 [272–491]; A/H3N2: 286 [233–352] vs 315 [257–386]; B/Yamagata: 429 [350–525] vs 471 [378–588]; B/Victoria: 377 [325–438] vs 390 [327–465] for the coadministration and QIV-HD groups, respectively). SARS-CoV-2 binding antibody geometric mean concentrations also increased to similar levels in the coadministration and mRNA-1273 groups at day 22 (7634 [95% CI 6445–9042] and 7904 [6883–9077], respectively).
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine
- Record: found
- Abstract: found
- Article: not found
Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data
- Record: found
- Abstract: found
- Article: not found
