- Record: found
- Abstract: found
- Article: found
Combination of neuron-specific enolase measurement and initial neurological examination for the prediction of neurological outcomes after cardiac arrest
Read this article at
Abstract
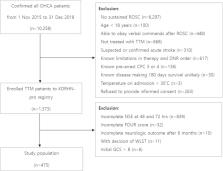
This study aimed to investigate the efficacy of the combination of neuron-specific enolase (NSE) measurement and initial neurological examination in predicting the neurological outcomes of patients with cardiac arrest (CA) by retrospectively analyzing data from the Korean Hypothermia Network prospective registry. NSE levels were recorded at 48 and 72 h after CA. The initial Full Outline of UnResponsiveness (FOUR) and Glasgow Coma Scale (GCS) scores were recorded. These variables were categorized using the scorecard method. The primary endpoint was poor neurological outcomes at 6 months. Of the 475 patients, 171 (36%) had good neurological outcomes at 6 months. The areas under the curve (AUCs) of the categorized NSE levels at 72 h, GCS score, and FOUR score were 0.889, 0.722, and 0.779, respectively. The AUCs of the combinations of categorized NSE levels at 72 h with categorized GCS scores and FOUR score were 0.910 and 0.912, respectively. Each combination was significantly higher than the AUC value of the categorized NSE level at 72 h alone (with GCS: p = 0.015; with FOUR: p = 0.026). Combining NSE measurement and initial neurological examination improved the prediction of neurological outcomes.
Related collections
Most cited references30
- Record: found
- Abstract: not found
- Article: not found
Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.
- Record: found
- Abstract: found
- Article: not found
Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.

- Record: found
- Abstract: found
- Article: found