- Record: found
- Abstract: found
- Article: found
Cohort profile: the Scottish Diabetes Research Network national diabetes cohort – a population-based cohort of people with diabetes in Scotland
Read this article at
Abstract
Purpose
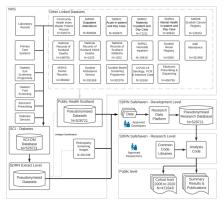
The Scottish Diabetes Research Network (SDRN)-diabetes research platform was established to combine disparate electronic health record data into research-ready linked datasets for diabetes research in Scotland. The resultant cohort, ‘The SDRN-National Diabetes Dataset (SDRN-NDS)’, has many uses, for example, understanding healthcare burden and socioeconomic trends in disease incidence and prevalence, observational pharmacoepidemiology studies and building prediction tools to support clinical decision making.
Participants
We estimate that >99% of those diagnosed with diabetes nationwide are captured into the research platform. Between 2006 and mid-2020, the cohort comprised 472 648 people alive with diabetes at any point in whom there were 4 million person-years of follow-up. Of the cohort, 88.1% had type 2 diabetes, 8.8% type 1 diabetes and 3.1% had other types (eg, secondary diabetes). Data are captured from all key clinical encounters for diabetes-related care, including diabetes clinic, primary care and podiatry and comprise clinical history and measurements with linkage to blood results, microbiology, prescribed and dispensed drug and devices, retinopathy screening, outpatient, day case and inpatient episodes, birth outcomes, cancer registry, renal registry and causes of death.
Findings to date
There have been >50 publications using the SDRN-NDS. Examples of recent key findings include analysis of the incidence and relative risks for COVID-19 infection, drug safety of insulin glargine and SGLT2 inhibitors, life expectancy estimates, evaluation of the impact of flash monitors on glycaemic control and diabetic ketoacidosis and time trend analysis showing that diabetic ketoacidosis (DKA) remains a major cause of death under age 50 years. The findings have been used to guide national diabetes strategy and influence national and international guidelines.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland
- Record: found
- Abstract: found
- Article: not found
Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008-2010.

- Record: found
- Abstract: found
- Article: found