- Record: found
- Abstract: found
- Article: found
Five-fraction CyberKnife radiotherapy for large brain metastases in critical areas: impact on the surrounding brain volumes circumscribed with a single dose equivalent of 14 Gy (V14) to avoid radiation necrosis
Read this article at
Abstract
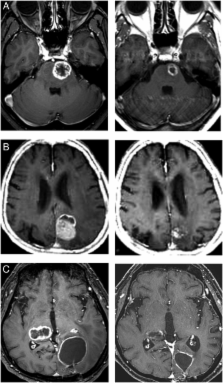
The efficacy and toxicity of five-fraction CyberKnife radiotherapy were evaluated in patients with large brain metastases in critical areas. A total of 85 metastases in 78 patients, including tumors >30 cm 3 (4 cm in diameter) were treated with five-fraction CyberKnife radiotherapy with a median marginal dose of 31 Gy at a median prescribed isodose of 58%. Changes in the neurological manifestations, local tumor control, and adverse effects were investigated after treatment. The surrounding brain volumes circumscribed with 28.8 Gy (single dose equivalent to 14 Gy: V14) were measured to evaluate the risk of radiation necrosis. Neurological manifestations, such as motor weakness, visual disturbances and aphasia improved in 28 of 55 patients (50.9%). Local tumor control was obtained in 79 of 85 metastases (92.9%) during a median follow-up of eight months. Symptomatic edema occurred in 10 patients, and two of them (2.6%) required surgical resection because of radiation necrosis. The V14 of these patients was 3.0–19.7 cm 3. There were 16 lesions with a V14 of ≥7.0 cm 3, and two of these lesions developed extensive brain edema due to radiation necrosis. None of the patients with a V14 of <7.0 cm 3 exhibited edema requiring surgical intervention. We therefore conclude that a high rate of local tumor control and low rates of complications can be obtained after five-fraction CyberKnife radiotherapy for large metastases in critical areas. The V14 of the surrounding brain is therefore a useful indicator for the risk of radiation necrosis in patients with large metastases.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials.
- Record: found
- Abstract: not found
- Article: not found
An overview of hypofractionation and introduction to this issue of seminars in radiation oncology.
- Record: found
- Abstract: found
- Article: not found