- Record: found
- Abstract: found
- Article: found
Pap Testing in a High-Income Country with Suboptimal Compliance Levels: A Survey on Acceptance Factors among Sicilian Women
Read this article at
Abstract
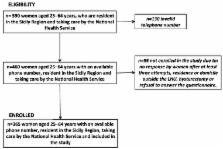
Cervical cancer screening is uncommon, especially in low-income countries and among lower socioeconomic status people in high-income countries. The aims of this study were to examine the adherence of Sicilian women to Pap testing and to identify the determinants of this in a population with a secondary prevention attitude lower than high-income countries and the national average. A cross-sectional study called “Save Eva in Sicily” was conducted among all women aged 25–64 years, with a sample drawn by the list of general practitioners (GPs), using a proportional sampling scheme, stratified by age and resident population. The study outcome was performing a Pap test within the past three years. The association between the outcome and Pap test determinants was analyzed through a multivariable logistic regression. Among the 365 interviewed women, 66% ( n = 243) had a Pap test during the last 3 years. On the other hand, 18% of the other women ( n = 66) had performed at least one Pap test previously and 16% ( n = 56) had never had a Pap test. In a multivariable model, GPs’ advice (adjusted OR 2.55; 95% CI 1.57–4.14) and perceived susceptibility (adjusted OR 3.24; 95% CI 1.92–5.48) increased the likelihood of the execution of a Pap test. The “Save Eva in Sicily” study identified GP advice and perceived cancer severity as the main correlates of Pap testing among Sicilian women, producing evidence regarding how policy makers can increase compliance. Interventions to increase Pap test adhesion should focus on stimulating GPs to identify patients who regularly do not undergo it and to recommend testing on a regular basis to their patients.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Impact of provider-patient communication on cancer screening adherence: A systematic review.
- Record: found
- Abstract: not found
- Article: not found
GLOBOCAN 2020: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2020
- Record: found
- Abstract: found
- Article: not found