- Record: found
- Abstract: found
- Article: found
Invasive breast carcinoma with ipsilateral axillary squamous carcinoma of unknown primary: A case report
Read this article at
Abstract
Introduction & importance
Invasive ductal carcinoma is the commonest primary breast carcinoma to metastasize to the axillary nodes. Squamous carcinoma (SCC) of the breast is seen rarely as a primary breast malignancy. Breast SCC with coexistent invasive ductal/lobular carcinoma as a ‘collision tumour’ is rare.
Case presentation
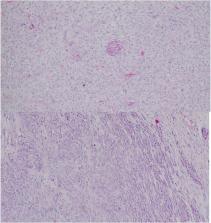
A 52-year-old Sri Lankan female presented with a right sided breast lump and ipsilateral cystic axillary mass. She was diagnosed with locally advanced invasive breast carcinoma and underwent neoadjuvant chemotherapy followed by mastectomy and axillary clearance where tumour infiltration of the brachial plexus was observed. Histology revealed two separate carcinomas; an invasive carcinoma of the breast and squamous carcinoma in the axilla. A squamous primary was not found despite evaluation. The patient developed recurrent axillary ulceration due to residual tumour and was transferred for oncological care.
Clinical discussion
This patient had a biopsy-proven invasive breast carcinoma with a cystic axillary mass with lymphadenopathy. This was concluded as locally advanced breast cancer. Pathological examination of the specimen indicated the presence of two separate malignancies of the breast and axilla. No evidence of squamous metaplasia or carcinoma of the breast was seen on histology, neither was a squamous primary identified on imaging or endoscopy. Neoadjuvant therapy may have caused resolution of the squamous component.
Highlights
-
•
Squamous cell carcinoma (SCC) of the breast is a rare primary breast cancer and metastasis of SCC to the breast is more common.
-
•
Invasive breast carcinoma has been described in combination with primary breast SCC and SCC of the breast skin as collision tumours.
-
•
Invasive breast carcinoma with SCC of unknown primary in the ipsilateral axilla as two separate distinct tumours has not been described before.