- Record: found
- Abstract: found
- Article: found
Estimating the impact of non-pharmaceutical interventions against COVID-19 on mumps incidence in Sichuan, China
Read this article at
Abstract
Background
A series of social and public health measures have been implemented to contain coronavirus disease 2019 (COVID-19) in China. We examined the impact of non-pharmaceutical interventions against COVID-19 on mumps incidence as an agent to determine the potential reduction in other respiratory virus incidence.
Methods
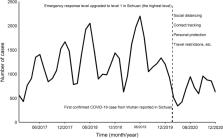
We modelled mumps incidence per month in Sichuan using a seasonal autoregressive integrated moving average (ARIMA) model, based on the reported number of mumps cases per month from 2017 to 2020.
Results
The epidemic peak of mumps in 2020 is lower than in the preceding years. Whenever compared with the projected cases or the average from corresponding periods in the preceding years (2017–2019), the reported cases in 2020 markedly declined ( P < 0.001). From January to December, the number of mumps cases was estimated to decrease by 36.3% (33.9–38.8%), 34.3% (31.1–37.8%), 68.9% (66.1–71.6%), 76.0% (73.9–77.9%), 67.0% (65.0–69.0%), 59.6% (57.6–61.6%), 61.1% (58.8–63.3%), 49.2% (46.4–52.1%), 24.4% (22.1–26.8%), 30.0% (27.5–32.6%), 42.1% (39.6–44.7%), 63.5% (61.2–65.8%), respectively. The total number of mumps cases in 2020 was estimated to decrease by 53.6% (52.9–54.3%).
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia
- Record: found
- Abstract: found
- Article: not found
Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study
- Record: found
- Abstract: found
- Article: not found