- Record: found
- Abstract: found
- Article: found
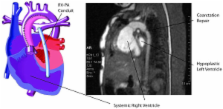
Cardiovascular magnetic resonance of pulmonary artery growth and ventricular function after Norwood procedure with Sano modification
Read this article at
Abstract
For hypoplastic left heart syndrome (HLHS), there have been concerns regarding pulmonary artery growth and ventricular dysfunction after first stage surgery consisting of the Norwood procedure modified with a right ventricle-to-pulmonary artery conduit. We report our experience using cardiovascular magnetic resonance (CMR) to determine and follow pulmonary arterial growth and ventricular function in this cohort.
Following first stage palliation, serial CMR was performed at 1 and 10 weeks post-operatively, followed by cardiac catheterization at 4 – 6 months. Thirty-four of 47 consecutive patients with HLHS (or its variations) underwent first stage palliation. Serial CMR was performed in 20 patients. Between studies, ejection fraction decreased (58 ± 9% vs. 50 ± 5%, p < 0.05). Pulmonary artery growth occurred on the left (6 ± 1 mm vs. 4 ± 1 mm at baseline, p < 0.05) but not significantly in the right. This trend continued to cardiac catheterization 4–6 months post surgery, with the left pulmonary artery of greater size than the right (8.8 ± 2.2 mm vs. 6.7 +/- 1.9 mm, p < 0.05). By CMR, 5 had pulmonary artery stenoses initially, and at 2 months, 9 had stenoses. Three of the 9 underwent percutaneous intervention prior to the second stage procedure.
In this cohort, reasonable growth of pulmonary arteries occurred following first stage palliation with this modification, although that growth was preferential to the left. Serial studies demonstrate worsening of ventricular function for the cohort. CMR was instrumental for detecting pulmonary artery stenosis and right ventricular dysfunction.
Related collections
Most cited references20
- Record: found
- Abstract: not found
- Article: not found
Physiologic repair of aortic atresia-hypoplastic left heart syndrome.
- Record: found
- Abstract: found
- Article: not found
Right ventricle-pulmonary artery shunt in first-stage palliation of hypoplastic left heart syndrome.
- Record: found
- Abstract: found
- Article: not found