- Record: found
- Abstract: found
- Article: not found
Crystalline lens changes in porcine eyes with implanted phakic IOL (ICL) with a central hole
Read this article at
Abstract
Background
We calculated the smallest diameter of a hole in the center of the optic at which the optical character of a phakic IOL (ICL) may be maintained. The changes induced in the aqueous humor dynamics and the pathology of cataract development with such a hole were investigated.
Methods
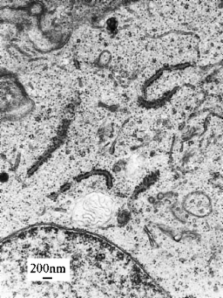
A simulation was performed using ZEMAX software to calculate the hole diameter that makes possible the maintenance of a stable optical character of a phakic IOL. After a hole of calculated diameter was trepanned in the center of the optic of the ICL, the latter was implanted into one eye of a 5-month-old minipig, and an unperforated ICL into the other. The postoperative course was observed for 3 months. Then, Evans blue was injected into the vitreous body under general anesthesia to stain the anterior capsule of the crystalline lens. Within 30 min, the eye was enucleated and the tissues removed were fixed.
Results
The MTF of the perforated ICL (hole diameter, 1.0 mm) in the center of the optic resembled that of the unperforated ICL. In all cases with non-perforated ICLs, subcapsular turbidity developed, but no staining caused by EB was observed in the anterior capsule. On the other hand, the anterior capsules of the eyes fitted with ICLs with a 1.0-mm hole were stained, but exhibited no turbidity.
Conclusion
An ICL with a central hole of diameter 1.0 mm in the optic is similar to an unperforated ICL. The size of the hole influenced the aqueous humor dynamics and increased the aqueous humor perfusion volume over the entire anterior surface of the crystalline lens. The possibility of preventing cataracts was therefore suggested.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
United States Food and Drug Administration clinical trial of the Implantable Collamer Lens (ICL) for moderate to high myopia: three-year follow-up.
- Record: found
- Abstract: found
- Article: not found
U.S. Food and Drug Administration clinical trial of the Implantable Contact Lens for moderate to high myopia.
- Record: found
- Abstract: found
- Article: not found
