- Record: found
- Abstract: found
- Article: found
Systematic identification of critically ill and dying patients in primary care using the German version of the Supportive and Palliative Care Indicators Tool (SPICT-DE) Translated title: Systematische Identifikation von schwerstkranken und sterbenden Patientinnen und Patienten in der Primärversorgung anhand der deutschsprachigen Version des Supportive and Palliative Care Indicators Tool (SPICT-DE)
Read this article at
Abstract
Objective: The systematic identification of patients who are at risk of deteriorating and dying is the prerequisite for the provision of palliative care (PC). This study aimed to investigate the feasibility and practicability of the German version of the Supportive and Palliative Care Indicators Tool (SPICT-DE) for the systematic identification of these patients in general practice.
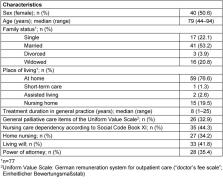
Methods: In the beginning of 2017, twelve general practitioners (GPs; female n=6) were invited to take part in the study. GPs were asked to apply the SPICT-DE in everyday practice over a period of two months in patients with chronic progressive diseases. Six months after initial assessment, a follow-up survey revealed how the clinical situation of the initially identified patients had changed and which PC actions had been initiated by GPs. In addition, GPs gave feedback on the practicability of SPICT-DE in daily routine.
Results: 10 of the 12 GPs (female n=5, median age 46 years, range 38–68) participated in both the two-month assessment period and the follow-up survey. A total of 79 patients (female n=40, median age 79 years, range 44–94) was assessed with the SPICT-DE. Main diagnoses were predominately of cardio-vascular (n=28) or oncological (n=26) origin. Follow-up after six months showed that 38 patients (48%) went through at least one crisis during the course of disease and almost one third (n=26) had died. The majority of GPs (n=7) considered the SPICT-DE to be practical in daily routine and helpful in identifying patients who might benefit from PC. Seven GPs indicated that they would use the SPICT-DE as part of everyday practice.
Conclusions: The SPICT-DE seems to be a practical tool supporting the systematic identification of critically ill and dying patients in general practice.
Zusammenfassung
Ziel: Die systematische Identifikation von Patientinnen und Patienten, bei denen eine Verschlechterung des Gesundheitszustandes und das Versterben abzusehen sind, ist die Voraussetzung für die Einleitung einer Palliativversorgung. Diese Studie untersucht die Anwendung und Praktikabilität der deutschen Version des Supportive and Palliative Care Indicators Tool (SPICT-DE) bei der systematischen Identifikation dieser Patientinnen und Patienten in der hausärztlichen Versorgungspraxis.
Methoden: Anfang 2017 wurden zwölf Hausärztinnen und Hausärzte (weiblich n=6) zur Teilnahme an der Studie eingeladen, um SPICT-DE in einem Zeitraum von zwei Monaten bei Patientinnen und Patienten mit chronisch progredienten Erkrankungen anzuwenden. Sechs Monate nach der ersten Anwendung wurde in einer Nacherhebung erfasst, wie sich der Gesundheitszustand dieser Patientinnen und Patienten im Verlauf geändert hat und welche palliativmedizinischen Maßnahmen durch die Hausärztinnen und Hausärzte in der Zwischenzeit eingeleitet wurden. Ergänzend haben die Hausärztinnen und Hausärzte einen Feedbackbogen zur Praktikabilität von SPICT-DE im Praxisalltag ausgefüllt.
Ergebnisse: Zehn der zwölf Hausärztinnen und Hausärzte (weiblich n=5, Altersmedian 46 Jahre, Spannweite 38–68) nahmen sowohl an der Anwendungsphase als auch an der Nacherhebung teil. Insgesamt 79 Patientinnen und Patienten (weiblich n=40, Altersmedian 79 Jahre, Spannweite 44–94) wurden mittels SPICT-DE beurteilt. Die Hauptdiagnosen waren vornehmlich aus dem kardiovaskulären (n=28) oder onkologischen Bereich (n=26). Die Nacherhebung sechs Monate nach der initialen Anwendung von SPICT-DE zeigte, dass bei 38 Patientinnen und Patienten (48%) mindestens ein krisenhaftes Ereignis im Krankheitsverlauf auftrat und dass fast ein Drittel (n=26) in der Zwischenzeit verstorben war. Die Mehrheit der Hausärztinnen und Hausärzte (n=7) erachteten SPICT-DE als praktikabel in der täglichen Anwendung und hilfreich bei der Identifikation von Patientinnen und Patienten, die von einer Palliativversorgung profitieren können. Sieben Hausärztinnen und Hausärzte gaben an, dass sie SPICT-DE auch zukünftig im Rahmen der hausärztlichen Versorgungspraxis nutzen würden.
Schlussfolgerungen: SPICT-DE scheint ein praktisches Instrument für die hausärztliche Versorgungspraxis zu sein, um schwerstkranke und sterbende Patientinnen und Patienten systematisch zu identifizieren.
Related collections
Most cited references20
- Record: found
- Abstract: not found
- Article: not found
Palliative Care: the World Health Organization's global perspective.
- Record: found
- Abstract: not found
- Article: not found
Development and evaluation of the Supportive and Palliative Care Indicators Tool (SPICT): a mixed-methods study

- Record: found
- Abstract: found
- Article: found