- Record: found
- Abstract: found
- Article: found
Experimental validation of the Eclipse AAA algorithm
Read this article at
Abstract
The present study evaluates the performance of a newly released photon‐beam dose calculation algorithm that is incorporated into an established treatment planning system (TPS). We compared the analytical anisotropic algorithm (AAA) factory‐commissioned with “golden beam data” for Varian linear accelerators with measurements performed at two institutions using 6‐MV and 15‐MV beams. The TG‐53 evaluation regions and criteria were used to evaluate profiles measured in a water phantom for a wide variety of clinically relevant beam geometries. The total scatter factor (TSF) for each of these geometries was also measured and compared against the results from the AAA.
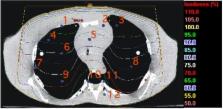
At one institute, TLD measurements were performed at several points in the neck and thoracic regions of a Rando phantom; at the other institution, ion chamber measurements were performed in a CIRS inhomogeneous phantom. The phantoms were both imaged using computed tomography (CT), and the dose was calculated using the AAA at corresponding detector locations. Evaluation of measured relative dose profiles revealed that 97%, 99%, 97%, and 100% of points at one institute and 96%, 88%, 89%, and 100% of points at the other institution passed TG‐53 evaluation criteria in the outer beam, penumbra, inner beam, and buildup regions respectively. Poorer results in the inner beam regions at one institute are attributed to the mismatch of the measured profiles at shallow depths with the “golden beam data.”
For validation of monitor unit (MU) calculations, the mean difference between measured and calculated TSFs was less than 0.5%; test cases involving physical wedges had, in general, differences of more than 1%. The mean difference between point measurements performed in inhomogeneous phantoms and Eclipse was 2.1% (5.3% maximum) and all differences were within TG‐53 guidelines of 7%. By intent, the methods and evaluation techniques were similar to those in a previous investigation involving another convolution–superposition photon‐beam dose calculation algorithm in another TPS, so that the current work permitted an independent comparison between the two algorithms for which results have been provided.
PACS number: 87.53.Dq
Related collections
Most cited references18
- Record: found
- Abstract: not found
- Article: not found
Comprehensive QA for radiation oncology: report of AAPM Radiation Therapy Committee Task Group 40.
- Record: found
- Abstract: found
- Article: not found
American Association of Physicists in Medicine Radiation Therapy Committee Task Group 53: quality assurance for clinical radiotherapy treatment planning.
- Record: found
- Abstract: found
- Article: not found