- Record: found
- Abstract: found
- Article: found
Clinical Characteristics and Outcome of Bloodstream Infections in HIV-Infected Patients with Cancer and Febrile Neutropenia: A Case–Control Study
Read this article at
Abstract
Introduction
We aimed to compare the clinical characteristics and outcomes of bloodstream infections (BSI) in cancer patients presenting febrile neutropenia with and without HIV infection, and analyze the prognostic factors for mortality.
Methods
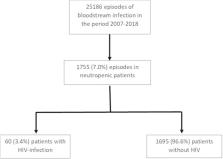
BSI episodes in febrile neutropenic patients following chemotherapy were prospectively collected (1997–2018). A case (HIV-infected)–control (non-HIV-infected) sub-analysis was performed (1:2 ratio), matching patients by age, gender, baseline disease, and etiological microorganism.
Results
From 1755 BSI episodes in neutropenic cancer patients, 60 (3.4%) occurred in those with HIV. HIV characteristics: 51.7% were men who have sex with men; 58.3% had < 200 CD4; 51.7% had a detectable HIV-1 RNA viral load before the BSI episode; 70.0% met AIDS-defining criteria; and 93.3% were on antiretroviral therapy, with a protease inhibitor-based regimen being the most common (53.0%). HIV-infected patients were younger, more frequently male and more commonly presenting chronic liver disease ( p < 0.001 for all). BSI due to Enterococcus spp. was significantly more frequent among patients with HIV ( p = 0.017) with no differences in other pathogens. HIV-infected patients with cancer presented with shock more frequently ( p = 0.014) and had higher mortality (31.7% vs. 18.1%, p = 0.008). In the case–control analysis, cases (HIV-infected) had chronic liver disease ( p = 0.003) more frequently, whereas acute leukemia ( p = 0.013) and hematopoietic stem-cell transplant ( p = 0.023) were more common among controls. There was a non-significant trend for cases to have higher mortality ( p = 0.084). However, in multivariate analysis, HIV infection was not associated with mortality ( p = 0.196).
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
Antimicrobial Resistance in Gram-Negative Rods Causing Bacteremia in Hematopoietic Stem Cell Transplant Recipients: Intercontinental Prospective Study of the Infectious Diseases Working Party of the European Bone Marrow Transplantation Group
- Record: found
- Abstract: found
- Article: not found
Risk of bacteraemia and mortality in patients with haematological malignancies.
- Record: found
- Abstract: found
- Article: not found