- Record: found
- Abstract: found
- Article: found
COVID-19 Induced Postural Orthostatic Tachycardia Syndrome (POTS): A Review
Read this article at
Abstract
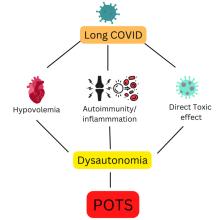
POTS (Postural Orthostatic Tachycardia Syndrome) is a multisystem disorder characterized by the abnormal autonomic response to an upright posture, causing orthostatic intolerance and excessive tachycardia without hypotension. Recent reports suggest that a significant percentage of COVID-19 survivors develop POTS within 6 to 8 months of infection. Prominent symptoms of POTS include fatigue, orthostatic intolerance, tachycardia, and cognitive impairment. The exact mechanisms of post-COVID-19 POTS are unclear. Still, different hypotheses have been given, including autoantibody production against autonomic nerve fibers, direct toxic effects of SARS-CoV-2, or sympathetic nervous system stimulation secondary to infection. Physicians should have a high suspicion of POTS in COVID-19 survival when presented with symptoms of autonomic dysfunction and should conduct diagnostic tests like the Tilt table and others to confirm it. The management of COVID-19-related POTS requires a comprehensive approach. Most patients respond to initial non-pharmacological options, but when the symptoms become more severe and they do not respond to the non-pharmacological approach, pharmacological options are considered. We have limited understanding and knowledge of post-COVID-19 POTS, and further research is warranted to improve our understanding and formulate a better management plan.
Related collections
Most cited references95
- Record: found
- Abstract: found
- Article: found
Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms
- Record: found
- Abstract: found
- Article: found
The neuroinvasive potential of SARS‐CoV2 may play a role in the respiratory failure of COVID‐19 patients
- Record: found
- Abstract: not found
- Article: not found