- Record: found
- Abstract: found
- Article: found
Secukinumab efficacy in reducing the severity and the psychosocial impact of moderate‐to‐severe psoriasis as assessed by the Simplified Psoriasis Index: results from the IPSI‐PSO study
Read this article at
Abstract
Background
The utility of the Simplified Psoriasis Index (SPI), a recently developed multidomain tool for assessing psoriasis, was investigated in a study assessing response to secukinumab.
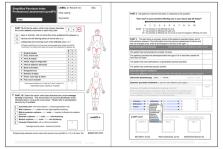
Methods
In an open‐label, multicentre study involving 17 French centres, patients with moderate‐to‐severe plaque psoriasis received secukinumab 300 mg subcutaneously once weekly from baseline to W4, then every 4 weeks until W48. Dermatologist‐scored SPI psoriasis severity (proSPI‐s) was compared with Psoriasis Area and Severity Index (PASI). Patient self‐assessed severity (saSPI‐s) and psychosocial impact (SPI‐p) were compared with PASI and Dermatology Life Quality Index (DLQI), respectively.
Results
We included 120 patients (69.2% male; mean age 45.9 years; mean duration of psoriasis 21.6 years). Mean baseline scores were as follows: proSPI‐s 24.9, saSPI‐s 23.5, PASI 23.1, SPI‐p 8.2 and DLQI 13.6. Severity scores achieved by 16 weeks (proSPI‐s 2.3, saSPI‐s 2.2 and PASI 2.2) were maintained to W52. Reductions in mean psychosocial impact scores were maintained to W52 (SPI‐p and DLQI, respectively, 2.1 and 1.5 at W16; 1.5 and 1.9 at W52).
Conclusions
Decrease of PASI scores in response to secukinumab was closely correlated with proSPI‐s, supporting the latter's suitability for assessing response to therapy. Although the correlation between PASI and saSPI‐s was slightly weaker, patients were able to complete a valid assessment of their psoriasis independently, and thus potentially remotely. With the added benefit of psychosocial impact assessment (SPI‐p), SPI provides a valid tool enabling patients to assess their own psoriasis, remotely if necessary.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Secukinumab in plaque psoriasis--results of two phase 3 trials.
- Record: found
- Abstract: found
- Article: not found
Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial.
- Record: found
- Abstract: found
- Article: not found