- Record: found
- Abstract: found
- Article: found
Finding covert fluid: methods for detecting volume overload in children on dialysis
Read this article at
Abstract
Background
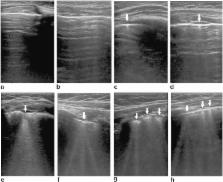
Lung ultrasound is a novel technique for detecting generalized fluid overload in children and adults with end-stage renal disease (ESRD). Echocardiography and bioimpedance spectroscopy are established methods, albeit variably adopted in clinical practice. We compared the practicality and accuracy of lung ultrasound with current objective techniques for detecting fluid overload in children with ESRD.
Methods
A prospective observational study was performed to compare lung ultrasound B-lines, echocardiographic measurement of inferior vena cava parameters and bioimpedance spectroscopy in the assessment of fluid overload in children with ESRD on dialysis. The utility of each technique in predicting fluid overload, based on short-term weight gain, was assessed. Multiple linear regression models to predict fluid overload by weight were explored.
Results
A total of 22 fluid assessments were performed in 13 children (8 on peritoneal dialysis, 5 on haemodialysis) with a median age of 4.0 (range 0.8–14.0) years. A significant linear correlation was observed between the number of B-lines detected by lung ultrasound and fluid overload by weight ( r = 0.57, p = 0.005). A non-significant positive linear correlation was observed between fluid overload by weight and bioimpedance spectroscopy ( r = 0.43, p = 0.2), systolic blood pressure ( r = 0.19, p = 0.4) and physical examination measurements ( r = 0.19, p = 0.4), while a non-significant negative linear relationship was found between the inferior vena cava collapsibility index and fluid overload by weight ( r = −0.24, p = 0.3). In multiple linear regression models, a combination of three fluid parameters, namely lung ultrasound B-lines, clinical examination and systolic blood pressure, best predicted fluid overload ( R 2 = 0.46, p = 0.05).
Conclusions
Lung ultrasound may be superior to echocardiographic methods and bioimpedance spectroscopy in detecting volume overload in children with ESRD. Given the practicality and sensitivity of this new technique, it can be adopted alongside clinical examination and blood pressure in the routine assessment of fluid status in children with ESRD.
Related collections
Most cited references29
- Record: found
- Abstract: not found
- Article: not found
Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography.
- Record: found
- Abstract: found
- Article: not found
Bioimpedance-guided fluid management in maintenance hemodialysis: a pilot randomized controlled trial.
- Record: found
- Abstract: found
- Article: not found