- Record: found
- Abstract: found
- Article: found
Awake craniotomies for aneurysms, arteriovenous malformations, skull base tumors, high flow bypass, and brain stem lesions
editorial
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Craniotomies for glioma resection under conscious sedation (CS) have been well-documented
in the literature for gliomas that are in or adjacent to eloquent areas.[1
2
3
4
5] To the best of our knowledge, based on a review of current literature, the use
of awake surgery forclipping of aneurysms, high flow extracranial to intercranial
(EC-IC) bypass, resection of arteriovenous malformations (AVMs), resection of skull
base tumors, and the resection of brain stem lesions has not previously been reported.
Intraoperative monitoring using electroencephalography (EEG), somatosensory evoked
potentials (SSEP), and motor evoked potentials (MEP) have inherent false-positives
and-negatives that have been reported and have been experienced by neurosurgeons during
craniotomies for the abovementioned pathologies.
During cerebral aneurysm surgery, temporary clipping is often required, and by proposing
craniotomy under CS, we are capable of assessing neurological function (i.e., hand-motor
function during middle cerebral artery division temporary clipping). At the final
reconstruction of the aneurysm and by assessing neurological function, we are able
to evaluate any potential risk to a perforator behind the aneurysm by performing a
direct neurological evaluation.
During microsurgical resection ofAVMs located in or around eloquent areas can be challenging.
This is due, in large part, to the risk of obliterating vessels in the area of the
AVM nidus that may be supplying normal cortical and subcortical structures. By checking
each one of these feeder versus bystander vessel by performing direct neurological
examination, we are able to avoid the risk of ischemia to normal brain tissue.
During high-flow EC-IC bypass surgery, two important steps, temporary occlusion of
the recipient vessel and the permanent occlusion of the parent aneurysmal vessel,
are monitored using electrophysiology, which can have both false-positives and -negatives.
The risk of the latter can be significantly avoided if the procedure can be performed
in a patient under conscious ("awake") sedation, allowing direct motor evaluation.
During brain stem surgery, monitoring technology is even more limited. By performing
the procedure under CS, we are able to test each function related to the respective
region being operated on and thus potentially decreasing the neurological morbidity
of the procedure.
Anesthesia team protocol is as follows: The surgical procedure is performed under
a monitored anesthesia care. Spontaneous respirations are maintained throughout the
case with dexmedetomidine (0.2-1.0 mcg/kg/h) and remifentanil (0.05-2 mcg/kg/min)
infusions. EEG monitoring is used to help gauge the appropriate depth of anesthesia.
A scalp block using 0.5% ropivicaine with epinephrine is used to anesthetize the respective
scalp region. Prior to the awake-phase of the surgery, thedexmedetomidineinfusion
is discontinued. Remifentanil is continued for pain control, and elevations in blood
pressure are treated with nitroglycerin and esmolol. Neurological evaluation is then
focused on the function of interest depending on the specific procedure. Sedation
is then restarted for the remainder of the surgery.
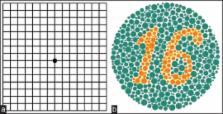
Motor function is tested for the respective region by a member of the neurosurgery
team. Vision testing is performed by using color plates and an iPad with specific
programs quantifying various visual tests [Figures 1 and 2]. Motor cranial nerve function
is tested directly.
Figure 1
Intraoperative photograph taken during temporary clipping of vessels surrounding a
pulvinar-occipital (arteriovenous malformation) AVM
Figure 2
(a) Amsler grid and (b) color plate
We have now performed 61 craniotomies using the above awake/CS protocol. No single
case had to be converted into general anesthesia during or after the procedure. Compared
to our own series prior to the awake procedures, for the same cases, we have lower
neurological morbidity, zero mortality, and shorter hospital stay in this cohort.
Related collections
Most cited references4
- Record: found
- Abstract: found
- Article: not found
Awake mapping optimizes the extent of resection for low-grade gliomas in eloquent areas.
- Record: found
- Abstract: found
- Article: not found
Awake craniotomy with brain mapping as the routine surgical approach to treating patients with supratentorial intraaxial tumors: a prospective trial of 200 cases.
Susan S. Taylor, Daniel M. Bernstein (1998)
- Record: found
- Abstract: found
- Article: not found
The predictive value of intraoperative somatosensory evoked potential monitoring: review of 244 procedures.
L Broemling, Elphège P Nora, Ghassan Bejjani … (1998)