- Record: found
- Abstract: found
- Article: found
Intrathecal Injection of Tigecycline and Polymyxin B in the Treatment of Extensively Drug-Resistant Intracranial Acinetobacter baumannii Infection: A Case Report and Review of the Literature
Read this article at
Abstract
Purpose
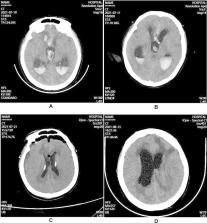
Intracranial infection after neurosurgery is one of the most serious complications, especially extensively drug-resistant (XDR) Acinetobacter baumannii ( A. baumannii) seriously affects the prognosis of patients. At present, there is little experience in the treatment of this infection and limited effective treatment options, like tigecycline or polymyxin B. Therefore, this report aims to describe the efficacy of tigecycline combined with polymyxin B by intrathecal (ITH) injection in the treatment of XDR intracranial infection with A. baumannii.
Methods
We report a case of intracranial infection with XDR A. baumannii after ventricular drainage, treated by daily ITH and intravenous (IV) tigecycline, combined with polymyxin B ITH route. Moreover, tigecycline and polymyxin B treatments for XDR intracranial infection with A. baumannii that were reported in the literature were also reviewed and summarized.
Related collections
Most cited references48
- Record: found
- Abstract: found
- Article: not found
International Consensus Guidelines for the Optimal Use of the Polymyxins
- Record: found
- Abstract: found
- Article: not found
Colistin in the 21st century.

- Record: found
- Abstract: found
- Article: found