- Record: found
- Abstract: found
- Article: found
Sclerosing angiomatoid nodular transformation (SANT) of the spleen: a case report with FDG-PET findings and literature review
Read this article at
Abstract
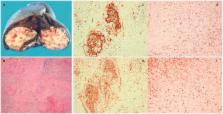
We report the 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) findings of sclerosing angiomatoid nodular transformation (SANT) of the spleen. The patient was a 37-year-old woman with a splenic mass incidentally found on abdominal ultrasound. FDG-PET/CT showed weak FDG accumulation (maximum standardized uptake value = 3.65). An unenhanced CT scan showed a low density and well-circumscribed splenic tumor that demonstrated weak enhancement from the arterial to delayed phase. Although hemangioma or hamartoma of the spleen was preoperatively diagnosed, histopathological examination revealed SANT. Therefore, when a splenic tumor with weak contrast medium enhancement and low FDG accumulation is observed, SANT should be considered as a differential diagnosis. Although CT and magnetic resonance imaging features of SANT have been reported, there are few reports on FDG-PET/CT findings. We report the radiological features of SANT, including FDG-PET/CT, and review the literature on SANT.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Sclerosing angiomatoid nodular transformation (SANT): report of 25 cases of a distinctive benign splenic lesion.
- Record: found
- Abstract: found
- Article: not found
Percutaneous image-guided biopsy of the spleen: systematic review and meta-analysis of the complication rate and diagnostic accuracy.
- Record: found
- Abstract: found
- Article: not found