Introduction
Coronary artery disease (CAD) is a common disease threatening human health. Coronary atherosclerosis (CA) is the most common mechanism of CAD. CA causes coronary artery stenosis and ischemia, thus leading to CAD or even acute myocardial infarction (AMI), the most serious complication of CAD. CAD without thrombosis is manifested by chronic stable angina as chronic coronary syndrome (CCS). CA, CCS and AMI are different stages of development of CAD.
Atherosclerosis is a passive lipid infiltration process, and inflammation plays an important role at every stage from atherosclerosis onset to progression to the development of thrombotic complications in atherosclerosis pathogenesis [1]. Atherosclerosis is an inflammatory process of the arteries, which is characterized by infiltration of immune cells, including monocytes, neutrophils and lymphocytes, thus leading to vascular wall degeneration in response to risk factors including hyperlipidemia, high blood pressure, high blood glucose levels and smoking [1]. Inflammation leads to the formation of plaques that can accelerate atherosclerotic progression, thereby causing CCS. When plaques erode or rupture, ACS can occur [2].
Among the markers of inflammation involved in atherosclerosis, white blood cell (WBC) subtypes play a key role in the progression of atherosclerosis and greatly increase the risk of thrombus formation and thrombotic events [3]. In sustained inflammation, neutrophils and monocytes increase, whereas lymphocytes decrease because of increased lymphocyte apoptosis [4]. In addition, ongoing inflammatory conditions produce megakaryocyte proliferation and increase platelet production [5].
Blood parameters such as the neutrophil/lymphocyte ratio (NLR), monocyte/lymphocyte ratio (MLR) and platelet/lymphocyte ratio (PLR) have been shown to be associated with inflammation and to be more accurate and stable than absolute blood cell counts [6]. Here, we aimed to perform a systematic comparison and assess the predictive values of these inflammatory parameters with CAD stage.
Methods
Study Population
The study was a single-center retrospective study. Clinical data for 513 patients who underwent coronary angiography (CAG) between June 2020 and January 2021 at the Second Affiliated Hospital of Chongqing Medical University were collected and analyzed. Patients with acute or chronic infection, autoimmune disease, congenital heart disease, chronic kidney failure, hematologic disease, liver or renal dysfunction, valvular disease, tumors, thyroid disease or chronic obstructive pulmonary disease, and patients without CAG were excluded from the study. Exclusion criteria also included age <18 years. According to the results of CAG, combined with clinical manifestations, and electrocardiographic and laboratory evaluations (particularly troponin T), the patients were divided into four groups: a normal coronary group, mild coronary atherosclerosis group (CA), CCS group and AMI group. The normal coronary group had normal CAG without any stenoses. In the CA group, patients had stenosis <50% diameter at angiography. The CCS group comprised patients with CAD without acute thrombotic events or myocardial damage. Patients in the AMI group had typical symptoms, electrocardiogram changes, and elevation of troponin T, and coronary artery lesions were identified by CAG. AMI included ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction, but excluded myocardial infarction with non-obstructive coronary arteries. CAD was defined as the existence of substantial narrowing (≥50%) in any main coronary arteries. Patient demographic data, such as age and sex, were recorded, and additional information including diabetes mellitus (DM), hypertension and smoking was gathered.
Laboratory Analysis
Lipid profiles and hematological parameters were measured by the clinical laboratory of the Second Affiliated Hospital of Chongqing Medical University.
Hematological Parameters
WBC, neutrophil count, lymphocyte count, monocyte count and platelet count were collected at admission. The NLR, MLR and PLR were calculated as the ratio between the total neutrophil and lymphocyte count; the total monocyte count and lymphocyte count, and the total platelet and lymphocyte count, respectively.
Lipid Profiles
Lipid profiles included low density lipoprotein cholesterol (LDL), high density lipoprotein cholesterol (HDL), total cholesterol (TC) and triglycerides (TG).
Statistical Analysis
Statistical analyses were performed in SPSS 20.0, software (IBM Corp., NY). Continuous variables were defined as mean±SD or median (interquartile range). Categorical variables are presented as percentages. For continuous variables, the Kolmogorov-Smirnov test was applied to test the normality assumption. According to the distribution pattern, Mann-Whitney U test or independent-sample t-test was used for continuous variables. For categorical variables, the chi-square test was used. One-way analysis of variance or Kruskal-Wallis test was used to compare the four groups. Then forced entry logicistic regression was used to evaluate the independent predictors of CAD (CCS and AMI). ROC curve analysis was used to verify the diagnostic accuracy of NLR, MLR and PLR levels in predicting the presence of different stages of CAD. A 2-tailed P value <0.05 was considered statistically significant.
Results
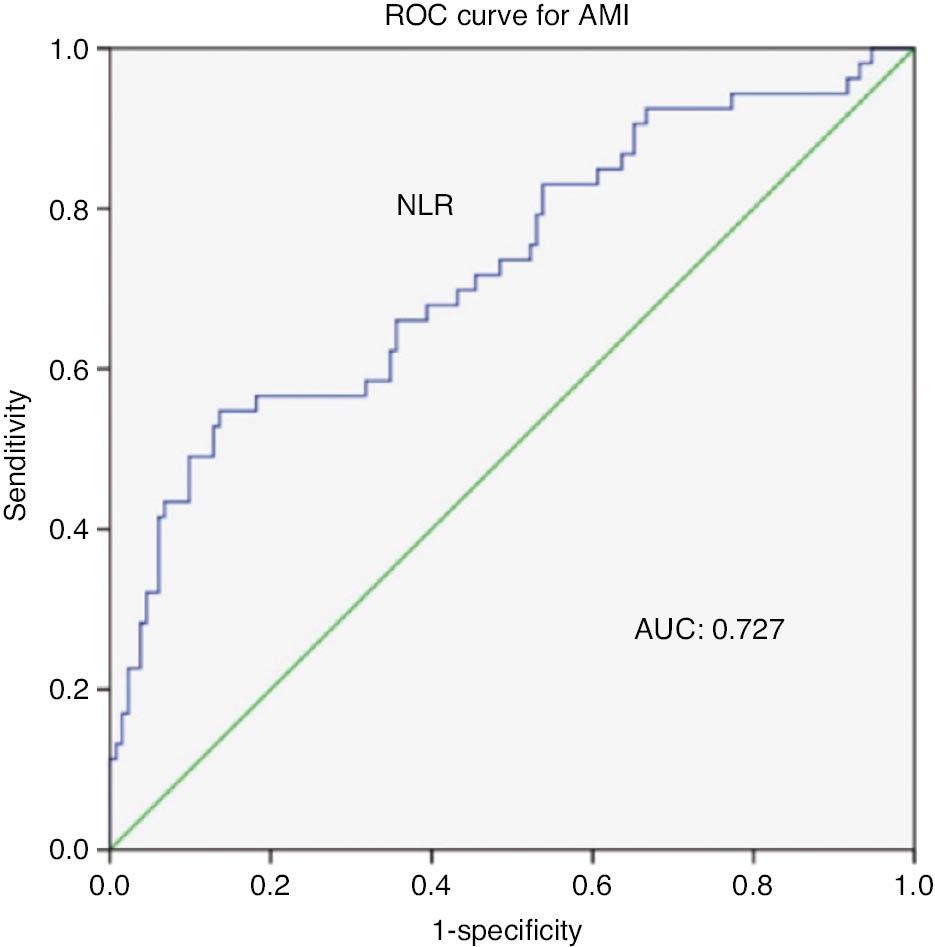
As shown in Table 1, 513 consecutive patients who underwent CAG and clinical evaluation were included in this study. The normal group consisted of 133 patients with normal angiography. The CA group included 149 patients. The CCS group consisted of 175 patients, and the AMI group consisted of 56 patients. The mean ages of patients in the CA group, CCS group and AMI group were older than that of patients in the normal group (P<0.001). Compared with that in the normal group, the prevalence of diabetes and hypertension was higher in the CA, CCS and AMI groups (P<0.05). The proportion of male patients and smokers was higher in the CCS and AMI groups than the normal and CA groups (P<0.05). No significant differences were observed in lipid profiles and hematological parameters between the CA group and the normal group (P>0.05). Moreover, no differences were observed in LDL levels among the four groups (P>0.05). The HDL level was lower in the CCS and AMI groups (P<0.001). Compared with the normal group, the CCS and AMI groups had higher neutrophil and monocyte counts. In addition, WBC counts were higher in the AMI group compared with the CCS group. Platelet levels did not differ among the 4 groups (P>0.05). NLR and MLR were higher in the CCS and AMI groups. PLR was higher in the AMI group. Meanwhile, in the AMI group, compared with the CCS group, NLR and PLR were higher (P<0.05). Figure 1 shows the unadjusted associations among NLR, PLR, MLR and different stages of CAD. Interestingly, patients with AMI presented markedly highest NLR, PLR and MLR. Logistic regression analysis was performed for conventional CAD risk factors (age, hypertension, DM and smoking); lipid factors (LDL and HDL); and NLR, MLR and PLR, to explore the independent risk factors for the development of CAD. As shown in Table 2, age, male sex, DM, smoking, LDL and NLR (B:1.227, 95% CI: 1.016–1.482, P<0.05) showed strong significant correlations with different developmental stages of CAD, whereas MLR and PLR did not. HDL appeared to be a protective factor among CAD patients.
Association between the (A) neutrophil-lymphocyte ratio (NLR), (B) monocyte-lymphocyte ratio (MLR), (C) platelet/lymphocyte ratio (PLR) and different stages of coronary artery disease (CAD).
Baseline Characteristics of the Study Population.
| Normal group (n=133) | CA group (n=149) | CCS group (n=175) | AMI group (n=56) | P | |
|---|---|---|---|---|---|
| Age (years) | 57(48,66.5) | 63(56,71)* | 67(59,73)*† | 66(58.2,5.72.75)*† | <0.001 |
| Male sex (%) | 62(46.6) | 81(54.4) | 119(68)*† | 40(71.4)*† | <0.001 |
| Coronary risk factors | |||||
| Hypertension, yes (%) | 51(38.3) | 73(49.3)* | 110(62.9)*† | 26(46.4)*† | <0.001 |
| Diabetes mellitus (%) | 16(12) | 30(20.3)* | 56(32)*† | 15(26.8)*† | <0.001 |
| Smoking, yes (%) | 40(30.1) | 44(29.7) | 68(38.9)*† | 30(53.6)*† | 0.005 |
| Lipid profile | |||||
| LDL (mmol/L) | 2.45±0.71 | 2.44±0.84 | 2.3±0.83 | 2.64±0.97 | 0.057 |
| HDL (mmol/L) | 1.17(1,1.36) | 1.19(1,1.41) | 1.06(0.92,1.23)*† | 1.04(0.85,1.18)*† | <0.001 |
| TC (mmol/L) | 4.52(3.78,5.29) | 4.58(3.9,5.42) | 4.29(3.6,5.04) | 4.34(3.62,5.25) | 0.054 |
| TG (mmol/L) | 1.36(0.93,1.89) | 1.35(0.96,2) | 1.36(0.98,1.84) | 1.52(1.13,2.12) | 0.631 |
| Hematologic parameters | |||||
| WBC (109/L) | 5.8(4.92,6.9) | 5.85(5,6.89) | 5.99(5.21,7.16) | 6.93(5.63,8.39)*†‡ | 0.001 |
| Neutrophils (109/L) | 3.61(3.08,4.54) | 3.74(2.98,4.81) | 3.8(3.2,4.79)* | 4.86(3.71,6.1)*†‡ | <0.001 |
| Lymphocytes (109/L) | 1.5(1.15,1.84) | 1.49(1.13,1.88) | 1.4(1.07,1.73) | 1.34(1.12,1.58) | 0.116 |
| Monocytes (109/L) | 0.4(0.3,0.49) | 0.39(0.29,0.51) | 0.45(0.35,0.55)*† | 0.47(0.4,0.59)*†‡ | <0.001 |
| Platelets (109/L) | 197.58±49.66 | 193.56±52.48 | 189.72±58.27 | 210.81±52.12 | 0.082 |
| NLR | 2.55(1.86,3.22) | 2.42(1.81,3.43) | 2.75(2.05,3.98)*† | 3.65(2.4,5.13)*†‡ | <0.001 |
| PLR | 130.18(97.85,167.66) | 127.27(98.13,173.18) | 132.94(102.89,176.52) | 149.45(123.26,220.67)*†‡ | 0.028 |
| MLR | 0.26(0.2,0.32) | 0.27(0.19,0.33) | 0.32(0.22,0.43)*† | 0.33(0.26,0.44)*† | <0.001 |
CA: coronary atherosclerosis; CCS: chronic coronary syndrome; AMI: acute myocardial infarction; LDL: low density lipoprotein cholesterol; HDL: high density lipoprotein cholesterol; TC: total cholesterol; TG: triglycerides; WBC: white blood cell; NLR: neutrophil/lymphocyte ratio; MLR: monocyte/lymphocyte ratio; PLR: platelet/lymphocyte ratio.
*Significantly different from the normal group.
†Significantly different from the CA group.
‡Significantly different from the CCS group.
Logistic Regression Analysis of Factors Independently Associated with CAD.
| Variables | Odds ratio | 95% Confidence interval | P | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 1.053 | 1.034 | 1.073 | <0.001 |
| Male sex | 1.593 | 1.044 | 2.430 | 0.031 |
| Hypertension, yes | 1.252 | 0.874 | 1.793 | 0.218 |
| DM, yes | 1.577 | 1.018 | 2.444 | 0.041 |
| Smoking | 1.6923 | 1.112 | 2.572 | 0.014 |
| HDL | 0.352 | 0.190 | 0.651 | 0.01 |
| LDL | 1.2419 | 1.005 | 1.532 | 0.044 |
| NLR | 1.227 | 1.016 | 1.482 | 0.033 |
| MLR | 0.945 | 0.141 | 6.315 | 0.954 |
| PLR | 0.999 | 0.995 | 1.003 | 0.716 |
DM: diabetes mellitus; HDL: high density lipoprotein cholesterol; LDL: low density lipoprotein cholesterol; NLR: neutrophil/lymphocyte ratio; MLR: monocyte/lymphocyte ratio; PLR: platelet/lymphocyte ratio.
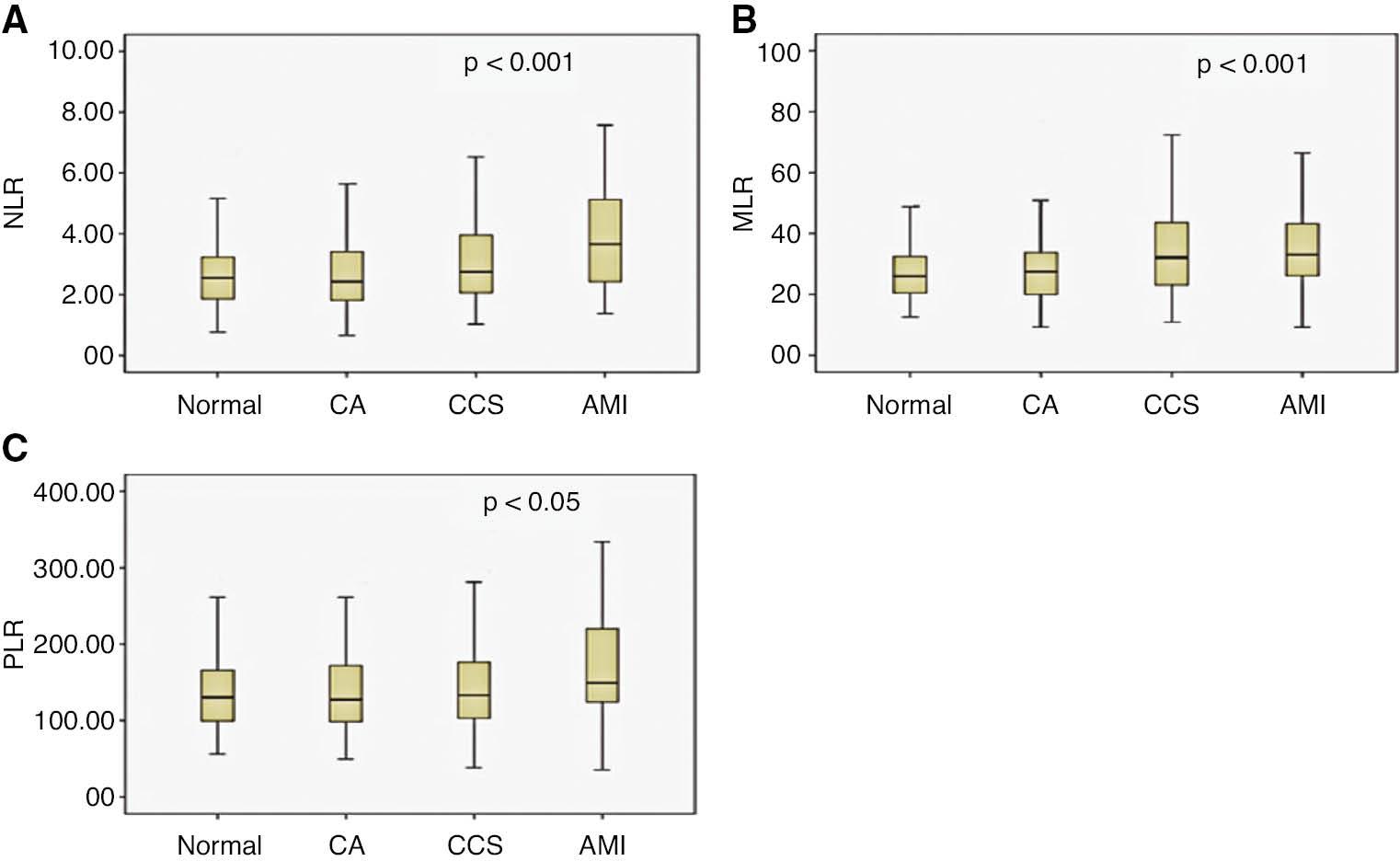
After adjustment for other factors, the area under the ROC curve of NLR in predicting CCS was 0.580 (95% CI=0.516–0.644, P<0.05) (Figure 2). The area under the ROC curve of NLR in predicting AMI was 0.727 (95% CI=0.642–0.811, P<0.001) (Figure 3).
Discussion
CAD is a frequently occurring disease with a high mortality rate. Straightening and obstruction of the coronary arteries from atherosclerosis are the main pathological changes. CAD is a multifactorial disease. Traditional risk factors, such as hyperlipidemia, hypertension, diabetes and smoking, are present in most patients with atherosclerosis and CAD. In our study, these risk factors were elevated in CA, CCS and AMI groups. Interestingly, our participants showed no difference in baseline LDL level, the most important known risk factor for CAD. This finding is likely to indicate that additional risk factors are involved in the formation of CAD.
Moreover, inflammation is associated with the development and progression of CAD [7].
Serum inflammatory markers, such as WBC count, neutrophils, lymphocytes, monocytes, platelets, NLR, MLR and PLR, play essential roles in the pathogenesis of atherosclerosis [3, 5, 8]. In this study, patients with CA did not show elevations in these inflammatory markers. Thus, we suggest that inflammation may not play an important role in the pathogenesis of mild atherosclerosis in CA, in which the degree of atherosclerosis is not sufficient to cause disease. However, the results of our study showed that inflammation was involved in the development of CCS and AMI.
This study revealed that patients with AMI had higher levels of inflammatory markers than those with CCS. The AMI group had higher WBC levels indicative of more severe inflammation. NLR is considered a marker of subclinical inflammation. In cases of sustained inflammation, neutrophil counts increase, and lymphocyte counts decrease, because of an increase in lymphocyte apoptosis secondary to physiological stress [9]. Neutrophils can increase damage to the endothelium, thus causing atherosclerosis [7].
According to recent studies, NLR is a powerful systemic inflammatory indicator associated with the prevalence and severity of CAD [10, 11]. Our study showed higher NLR levels in CAD, including CCS and particularly AMI. After AMI, myocardial necrosis initiates an inflammatory response through the recruitment of neutrophils and macrophages [12]. Thus, the elevated NLR may not only be associated with risk factors but also may include effects of myocardial necrosis. Overlapping effects may be possible. Our results indicated that NLR may be associated with the severity of CAD and may be considered a predictor of CCS progression to AMI.
Monocytes are also involved in endogenous inflammatory processes [13]. MLR is an inflammation marker widely used to assess the prognosis of cancer, tuberculosis, and autoimmune diseases. Recently, MLR has also been reported to be associated with cardiovascular events in patients with CAD [14–16]. In our study, the number of peripheral blood monocytes and the MLR level were elevated in both the CCS and AMI groups. However, in multivariate analysis, MLR was not found to be an independent risk factor, in contrast to Hanhua’s results [14]. In our study, NLR was more associated with CAD than MLR, thus indirectly indicating that neutrophils may play more important roles in the initiation and progression of atherosclerotic plaques than monocytes.
Persistent inflammation produces megakaryocyte proliferation and increase platelet production. Platelet activation is implicated in the pathophysiology of diseases prone to thrombosis and inflammation [17]. PLR is a marker that reflects both the aggregation status and inflammation pathway status [18]. The inflammatory response induced by platelets plays a key role in the occurrence and development of atherosclerosis [19]. PLR may be more valuable than either platelet or lymphocyte counts alone in the prediction of CAD, because it reveals the inflammatory and prothrombotic state. In this study, PLR levels were significantly elevated in the AMI group and were associated with AMI, an effect not found in the CCS group. Platelets are primarily involved in acute thrombotic events and are used as a marker to predict prothrombotic potential. In patients with CCS in our study, platelets and PLR levels did not increase, thus indicating that platelets have little effect on stabilizing CAD such as CCS, mainly because platelet aggregation was not discernible in CCS. Increased PLR values may be as a valuable predictor of the development of AMI rather than CCS.
Our study has several limitations. First, other inflammatory markers, such as C-reactive protein, interleukin-6 and tumor necrosis factor-alpha, were not measured in the study. Second, whether certain drugs with anti-inflammatory effects, including aspirin, statins or beta-blockers, might have influenced the inflammatory status is unknown.