Background
Severe left main coronary artery (LM) bifurcation lesions reduce most of the blood flow in the myocardium, leading to serious adverse cardiac events [1]. Coronary artery bypass grafting (CABG) has always been the preferred method for treating LM disease [2].
With the improvement of interventional techniques and stents, percutaneous coronary intervention (PCI) has proved feasible in the treatment of unprotected LM bifurcation lesions, and relevant studies have confirmed that there is no difference between PCI and CABG in the composite end point of death, cerebrovascular accident, and myocardial infarction during treatment [3, 4]. Therefore, PCI can be used as an effective and less invasive alternative to CABG.
In clinical settings, unprotected LM bifurcation lesions are treated mainly with single stenting or double stenting. Studies have confirmed that single stenting is superior to double stenting in clinical outcomes, but in about a third of cases a second stent still has to be implanted into branch vessels in many circumstances [5, 6]. Double stenting for treatment of LM bifurcation lesions is characterized by a long operation time, a high restenosis rate, and a high incidence of adverse cardiovascular events, which is not beneficial for the long-term prognosis of patients [7]. In recent years, a drug-coated balloon (DCB) has been widely recognized as a new interventional therapy in the treatment of in-stent restenosis [8]. The 2014 European Society of Cardiology guidelines recommend DCB as the preferred strategy for the treatment of in-stent restenosis [9]. Use of a DCB combined with a drug-eluting stent (DES) has the advantage of shortening the length of permanent metallic cages to reduce restenosis rates [10]. In terms of LM bifurcation lesions, researchers in China and elsewhere have also reported individual cases indicating that combined DES and DCB treatment can effectively reduce the restenosis rate in interventional therapy [11].
Method
A retrospective analysis was conducted for eight patients with LM bifurcation lesions treated with a DES combined with a DCB who were admitted to our hospital from July 2016 to July 2017. Demographics, DCB procedures, and quantitative coronary angiography (preoperative, postoperative, and 6-month follow-up) were reviewed. The LM bifurcation lesions selected in this work meet the requirements of left anterior descending coronary artery (LAD) and left circumflex artery (LCX) lesions, the degree of stenosis was more than 70%, and the LM was involved.
Results
Patients
This study enrolled eight patients (five female and three male) with an average age of 71.3 years, including four patients with unstable angina, four patients with stable angina, six patients with a history of hypertension, and three patients with diabetes (Table 1).
General and Arteriography Information for the Eight Patients.
| Parameter | Value |
|---|---|
| Age (years) | 71.3 ± 7.1 |
| Female sex (n) | 5 (62.5%) |
| Smoker (n) | 0 (0%) |
| Unstable angina (n) | 4 (50%) |
| Hypertension (n) | 6 (75%) |
| Diabetes (n) | 3 (37.5%) |
| Creatinine (μmol/L) | 102.8 ± 49.9 |
| Blood glucose (mmol/L) | 5.9 ± 2.3 |
| Glycated hemoglobin (%) | 6.4 ± 1.1 |
| LVEF (%) | 58.3 ± 6.5 |
LVEF, left ventricular ejection fraction.
DES and DCB Procedures
The eight patients all underwent DES treatment for their LM and LAD lesions, and DCB treatment at the ostium of the LCX. The operation involved the following procedures: placement of a working guide wire in the LCX and LAD, respectively, and predilation of the two blood vessels with a common balloon; implantation of a DCB into the LCX when the vascular stenosis had been adequately dilated (stenosis less than 50%), with an average dilation time of 60 s, and eventually implantation of a DES into the LAD, with an average dilation time of 10 s; withdrawal of the guide wire in the LCX, insertion of another guide wire through the mesh, and simultaneous dilation of the bifurcation lesions with the double-balloon kissing technique.
Quantitative Coronary Angiography
The dilation effect at LM, LAD, and LCX lesions in terms of stenosis diameter ratio (SDR), stenosis area ratio (SAR), and minimum lumen diameter (MLD) was maintained well by quantitative coronary angiography (Figure 1).
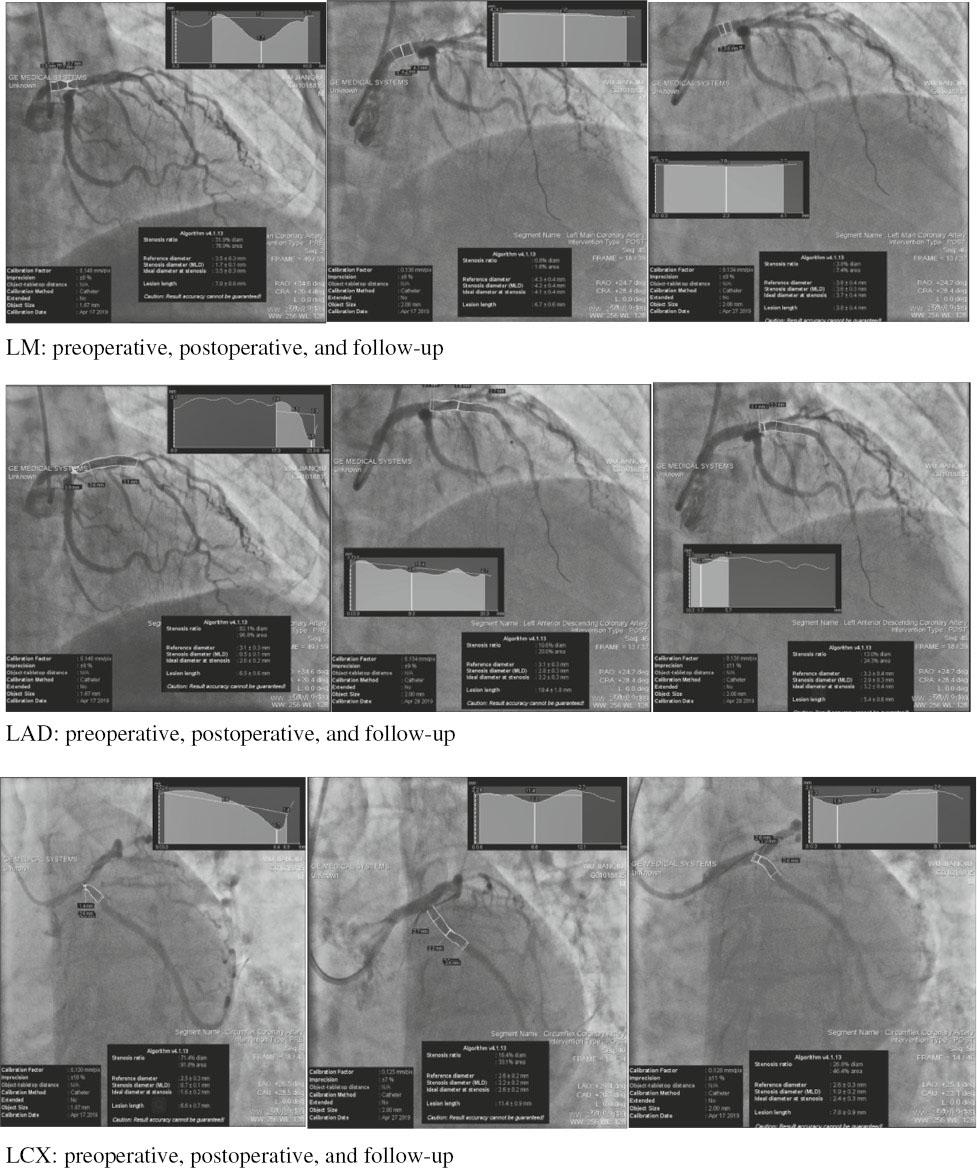
Angiographic Images of a Study Participant Preoperatively (left), Postoperatively (center), and at Follow-up (right): Left Main Coronary Artery (top), Left Anterior Descending Coronary Artery (middle), and Left Circumflex Artery (bottom).
The SDR and SAR were significantly lower and the MLD was significantly higher both postoperatively and at the 6-month follow-up than preoperatively (P<0.05; Table 2). These parameters were similar postoperatively and at the 6-month follow-up (P>0.05; Table 2), suggesting a low degree of restenosis after coronary intervention.
Comparison of Preoperative, Postoperative, and 6-Month Follow-Up Angiographic Results (n=8).
| Preoperative | Postoperative | 6-month follow-up | |
|---|---|---|---|
| LM | |||
| SDR (%) | 35.9 ± 25.1 | 6.2 ± 4.2* | 8.4 ± 5.3†,‡ |
| SAR (%) | 52.6 ± 31.9 | 11.9 ± 7.8* | 15.8 ± 9.5†,‡ |
| MLD (mm) | 2.4 ± 1.1 | 3.8 ± 0.4* | 3.5 ± 0.3†,‡ |
| LL (mm) | 5.8 ± 2.0 | ||
| LAD | |||
| SDR (%) | 79.7 ± 6.2 | 14.7 ± 3.0* | 18.2 ± 5.0†,‡ |
| SAR (%) | 95.5 ± 2.4 | 27.2 ± 5.0* | 32.3 ± 8.5†,‡ |
| MLD (mm) | 0.5 ± 0.2 | 2.8 ± 0.3* | 2.7 ± 0.4†,‡ |
| LL (mm) | 19.6 ± 11.2 | ||
| DESS (mm) | 3.3 ± 0.2 | ||
| EP (atm) | 11.1 ± 1.3 | ||
| LCX | |||
| SDR (%) | 87.1 ± 9.0 | 19.8 ± 10.6* | 30.5 ± 16.5†,‡ |
| SAR (%) | 97.2 ± 2.6 | 34.6 ± 16.6* | 49.0 ± 19.5†,‡ |
| MLD (mm) | 0.3 ± 0.2 | 1.8 ± 0.4* | 1.5 ± 0.4†,‡ |
| LL (mm) | 8.5 ± 4.0 | ||
| DCBS (mm) | 2.6 ± 0.3 | ||
| EP (atm) | 9.9 ± 2.4 | ||
Values are give as the mean ± standard deviation.
DCBS, drug-coated balloon size; DESS, drug-eluting stent size; EP, expansion pressure; LAD, left anterior descending coronary artery; LCX, left circumflex artery; LL, lesion length; LM, left main coronary artery; MLD, minimum lumen diameter; SAR, stenosis area ratio; SDR, stenosis diameter ratio.
*In the comparison of preoperative and postoperative results, P<0.05.
†In the comparison of preoperative and 6-month follow-up results, P<0.05.
‡In the comparison of postoperative and follow-up results, P>0.05.
Intravascular Ultrasonography Results
Six patients underwent preoperative and postoperative intravascular ultrasonography (IVUS) (Figure 2). The results showed that at LM, LAD, and LCX lesions, the minimum lumen area and MLD postoperatively were significantly higher than preoperatively (P<0.05; Table 3).

Intravascular Ultrasonography Images of a Study Participant Preoperatively (left) and Postoperatively (right): Left Main Coronary Artery (top), Left Anterior Descending Coronary Artery (middle), and Left Circumflex Artery (bottom).
Comparison of Preoperative and Postoperative Intravascular Ultrasonography Results (n=6).
| Preoperative | Postoperative | |
|---|---|---|
| LM | ||
| MLA (mm2) | 5.1 ± 0.6 | 10 ± 0.7* |
| MLD (mm) | 2.6 ± 0.3 | 3.3 ± 0.1* |
| LAD | ||
| MLA (mm2) | 2.7 ± 0.8 | 8 ± 1.0* |
| MLD (mm) | 1.6 ± 0.2 | 3 ± 0.2* |
| LCX | ||
| MLA (mm2) | 2.6 ± 0.3 | 4.2 ± 1.1* |
| MLD (mm) | 1.6 ± 0.1 | 2.1 ± 0.3* |
Values are give as the mean ± standard deviation.
LAD, left anterior descending coronary artery; LCX, left circumflex artery; LM, left main coronary artery; MLA, minimum lumen area; MLD, minimum lumen diameter.
*In the comparison of preoperative and postoperative results, P<0.05.
Discussion
LM bifurcation lesions belong to a type of high-risk and complex lesions in coronary interventional therapy, and CABG is initially preferred for the treatment of LM bifurcation lesions. In recent years, in studies comparing CABG and PCI in the treatment of LM bifurcation lesions, it has been found that there is no difference between the two in clinical prognosis during long-term follow-up [3, 4], and that PCI has a lower surgical risk in the treatment of the LM, but long-term follow-up shows a high angiographic restenosis rate, a high re-revascularization rate, and high incidence of cardiac death [12]. The development of the DES is a major breakthrough in the treatment of LM bifurcation lesions with PCI. Compared with the original bare metal stent, this stent can significantly reduce the occurrence of in-stent restenosis and re-revascularization of target lesions [13, 14].
Although interventional therapy with a first-generation DES can largely reduce the occurrence of in-stent restenosis, the cumulative incidence of late and very late stent thrombosis has been revealed [15], which is also an important factor for the poor long-term prognosis of early interventional therapy for LM bifurcation lesions. With the improvement of stents, the second-generation DES has more advantages in reducing the occurrence of stent thrombosis compared with the first-generation DES [16, 17]. A recent clinical trial for treatment of LM bifurcation lesions with the new-generation DES showed no significant difference in long-term outcomes compared with CABG because of its lower incidence of stent thrombosis and rapid endothelialization [18].
For LM true bifurcation lesions, the current PCI therapy in clinical settings is still primarily single-stenting or double-stenting intervention, but these two methods do not reduce the incidence of in-stent restenosis, possibly due to factors such as vascular anatomy (the proximal lesion involves longer vessel length and a wider angle of division), hemodynamics (large local blood flow), stent deformation, and reduced drug coverage [19–22]. Among these, stent thrombosis after single stenting may be caused by the protrusion of stent struts in the bifurcation lesion [23], and single stenting applies only for stent placement in the LM or LAD, while the LCX will be subject to plaque compression after stenting to various degrees, resulting in aggravated stenosis, which might eventually lead to total LCX occlusion. In contrast, double-stenting intervention involves stent placement in both the LAD and the LCX to recover patency of blood vessels, but since stents are placed in both blood vessels, the stent placement procedure is complicated, and the LM has a large bifurcation angle, which may cause the stent wire to become trapped at the bifurcation of the LM, greatly influencing blood flow and damaging blood vessels, and affecting stent endothelialization. In patients with LM bifurcation disease, the single-stent strategy showed a lower rate of major adverse cardiovascular events and target lesion revascularization, but in terms of cardiovascular mortality, target lesion failure, and stent thrombosis, it was not superior to the two-stent strategy at the 1-year follow-up and the 3-year follow-up [24].
Compared with conventional interventional therapy guided by angiography, IVUS-guided PCI can reduce long-term mortality associated with unprotected LM stenosis [25, 26]. IVUS can be used to identify the proximal and distal reference points and measure the distance between the two points to better determine the complexity of the lesion and select the appropriate stent diameter and length, thereby avoiding placing the edge of the stent into plaque. In addition, it is also possible to evaluate the stent apposition after stenting, so as to further increase the efficacy of stent implantation and optimize the final outcomes [27].
The biggest challenge in using a DES combined with a DCB for interventional physicians may be the occurrence of serious coronary artery dissection events after DCB treatment, but relevant studies have found that the incidence of such complications is just 5.9%, and the prognosis during long-term follow-up is good [28, 29]. Therefore, a DES combined with a DCB for treatment of LM bifurcation lesions may be a safe and effective new interventional therapy. In this study of the effectiveness and safety of combined DES and DCB treatment, angiography indicated that the SDR, SAR, and lesion length were significantly decreased and the MLD was significantly increased compared with preoperative values. At the 6-month follow-up, there was no significant difference in the SDR, SAR, lesion length, and MLD compared with the postoperative period. The results indicate that the DES and DCB method is effective, the rate of restenosis is low, and there are no adverse events such as major adverse cardiovascular events, target lesion revascularization, or target lesion failure after surgery, which may be attributed to the application of the new type of DES, the guidance by IVUS in the operation for LAD lesions, and the combination with a DCB for treatment of LCX lesions, which can effectively reduce the occurrence of LCX restenosis and reduce the adverse consequences of double stenting. During the 6-month follow-up, all patients received aspirin and clopidogrel daily for secondary prevention. Meanwhile, all patients were followed up for serious clinical events; all the patients had no stent thrombosis, myocardial infarction, cerebrovascular accident, target lesion revascularization, or cardiogenic death, further proving the safety of the combined DCB and DES treatment. This also shows that DCB treatment not only has advantages in small vessel diseases [30] but can also be applied to large vessel lesions such as LM bifurcation lesions.
Conclusions
Our study shows that the use of combined DES and DCB treatment has favorable outcomes at the 6-month follow-up for LM bifurcation lesion vascular reconstruction, the restenosis rate is significantly reduced, and there is a certain degree of effectiveness and safety. However, because of the small number of cases in this study, large-scale randomized controlled trials and longer-term follow-up are needed in the future to further demonstrate the effectiveness and safety of this strategy.

