Introduction
Severe aortic stenosis (AS) is a common condition in older people, with a prevalence of approximately 10% in individuals ≥80 years of age [1]. Interventional treatments, including conventional surgical aortic valve replacement (SAVR) and the a less invasive procedure of transcatheter aortic valve replacement (TAVR), have been demonstrated to achieve symptom improvement and survival benefits in symptomatic patients with severe AS [2, 3]. In recent decades, TAVR has shown comparable safety and efficacy to SAVR in managing this condition, regardless of surgical risk [4–10]. Consequently, the number of patients undergoing TAVR for severe AS is increasing, and the average patient age is approximately 80 years [11, 12]. The effects of advanced age on the clinical outcomes of TAVR patients are inconsistent, on the basis of various registry analyses and population studies across Europe and the United States [13–17]. Most of those studies involved patients with high surgical risk, thus potentially resulting in poorer clinical outcomes than might occur in patients with intermediate surgical risk [17]. However, some analyses have suggested, that compared with the Western population, the population of patients with aortic stenosis in Asia has a higher prevalence of bicuspid aortic valve (BAV) and a smaller aortic annulus size [18, 19]. Limited studies have evaluated the effects of age on TAVR in the older Asian population. Therefore, we conducted this study to analyze the effects of age on short-term (30-day) and 1-year clinical outcomes in Vietnamese patients with severe AS and intermediate surgical risk, comparing results between patients <80 and ≥80 years of age who underwent TAVR at a single center.
Methods
Study Design
This was a retrospective data analysis from a study evaluating the early safety and mid-term effectiveness of TAVR in the treatment of severe AS in the Vietnamese population. The patients were divided into two groups (<80 years old and ≥80 years old) to analyze the differences in clinical characteristics, procedures, and outcomes at the follow-up timepoints. The Ethical Review Board of The University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam, approved this study.
Setting
Between March 2017 and December 2022, 90 symptomatic patients with severe AS (defined by a mean transaortic pressure gradient >40 mmHg and aortic valve area <1.0 cm2) with NYHA >2 underwent TAVR at the Vinmec Central Park International Hospital in Ho Chi Minh City, Vietnam. Patients were examined, and the intervention strategy was determined by a heart team comprising specialists in cardiology, gerontology, interventional cardiology, cardiac surgery, anesthesia, and diagnostic imaging. The final decision to proceed with TAVR was made by the patients after consultation with the heart team. The patients’ intermediate surgical risk was assessed with the Society of Thoracic Surgeons (STS) score. The study was aimed at evaluating and comparing the clinical characteristics, procedures, and outcomes at 30 days and 1 year between two age groups: >80 and <80 years old.
Participants
We continuously collected all patients with severe AS at moderate surgical risk undergoing TAVR at the Vinmec Central Park International Hospital between March 2017 and the end of December 2022. The primary exclusion criteria were patients who had experienced acute myocardial infarction within the prior 3 months, stroke within the prior 6 months, severe heart failure with LVEF <20%, concomitant heart conditions requiring open-heart surgery, or active bleeding or infection; patients with a life expectancy less than 1 year; and patients with a mean aortic valve annulus diameter <18 mm or >30 mm. For patients transitioning to SAVR during follow-up, we ceased recording outcomes from the time of aortic valve replacement surgery. Patients were reassessed at 1 month, 3 months, and 1 year postoperatively. If patients missed their scheduled follow-up appointments, we communicated with patients/family members via telephone. If we cannot contact the patient or their relatives to obtain the necessary research information, we consider the patient lost to follow-up.
Study Procedures
All patients underwent TAVR in a hybrid operating room. New-generation self-expanding valve systems from Medtronics (Evolut R/Pro) were predominantly used, and only one patient received a balloon-expandable valve system (Sapien 3, Edwards). All patients underwent transthoracic echocardiography, coronary angiography, and evaluation of the aortic valve complex and vascular system by MSCT. Additionally, routine preoperative blood tests were conducted.
During the initial phase, most patients were induced under general anesthesia assisted with transesophageal echocardiography. Subsequently, we transitioned to a standard procedure with local anesthesia and without transesophageal echocardiography. Temporary ventricular rapid pacing was induced during the procedure through a pacing lead in the right ventricle in most cases, along with pacing via a guidewire to deliver the prosthesis valve in the left ventricle in recent cases.
Femoral arteries were used primarily for valve implantation, and alternative approaches (subclavian/axillary or carotid artery) were considered when the femoral route was deemed unsuitable for TAVR. Vascular closure devices were used for patients undergoing TAVR through femoral access. Pre-dilation was used primarily for patients with BAV with heavy calcification. In cases with extreme horizontal aorta, a snare was used to assist in advancing the Evolut R/Pro valve system through the aortic route.
Coplanar view was initially the preferred technique for achieving an optimal view to implant the prosthesis aortic valve, and was followed by the cusp-overlap technique. In all patients, the mean transaortic pressure gradient was measured before and immediately after prosthesis valve deployment. Aortic regurgitation was assessed postoperatively through aortic root angiography, echocardiography, and calculation of the Aortic Regurgitation Index.
All patients were temporarily maintained with a pacemaker for 24–48 hours postoperatively in the event of atrioventricular or left bundle branch block.
Data Variables
All basic patient characteristics, TAVI procedures and outcomes, and outcomes for assessing the early safety and 1-year clinical effectiveness of TAVI were documented for analysis. The clinical outcomes were defined in accordance with the Valve Academic Research Consortium (VARC)-2 criteria [20].
Study Sample Size
This study had a limited pool of eligible patients available for analysis, because of the condition’s rarity, and relied on data from the study titled “Early safety and mid-term clinical outcomes of technology transfer of transcatheter aortic valve implantation in patients with severe aortic valve stenosis in Vietnam: a single-center experience of 90 patients”. Consequently, a formal sample size calculation was not performed. Instead, we conducted an exhaustive analysis of all available patients meeting the inclusion criteria to ensure the maximal inclusion of cases, thereby optimizing the statistical power within the data availability constraints.
Statistical Analysis
Descriptive statistical analysis was performed for the different age groups, and the results are presented as mean ± standard deviation for continuous variables, and as number (%) for categorical variables. The Wilcoxon rank-sum test and Fisher’s exact test were used to compare continuous and categorical variables, respectively, between groups. The survival rate was estimated with the Kaplan-Meier method, and the log-rank test was used to compare groups. Clinical changes, including LVEF, mean transaortic pressure gradient, and NYHA classification, were illustrated in plots at various time points, including baseline, discharge, 30 days, and 12 months. Two-tailed statistical tests were used, with a significance level set at P < 0.05. The analysis used R statistical software version 4.1.0.
Results
Baseline Characteristics
Among the 90 patients with severe AS with symptoms and intermediate surgical risk who underwent TAVR at our hospital, 21 patients (23.3%) were ≥80 years old, and 69 patients were <80 years old. In the ≥80 year age group, 20 and 17 patients had a sufficient follow-up duration of 30 days and 1 year, respectively. Correspondingly, in the <80 year age group, 68 and 54 patients had a sufficient follow-up duration of 30 days and 1 year, respectively. The ≥80 year age group had a higher proportion of men (66.7%), whereas the sex distribution was approximately equal in the <80 year age group. Compared with the <80 year age group, the ≥80 year age group had a higher prevalence of comorbidities such as dyslipidemia, prior myocardial infarction, coronary artery disease with stent placement, cerebrovascular disease, and chronic obstructive pulmonary disease. The STS surgical risk score (6.1 ± 1.2 vs. 5.7 ± 1.0) and the proportion of NYHA III-IV heart failure (76.2% vs. 89.9%) did not significantly differ between groups. No significant differences were observed in the main echocardiographic and CT characteristics of the aortic valve region between patient groups, although the <80 year age group had a higher proportion of BAV (50.7% vs. 28.6%), whereas the ≥80 year age group had a higher proportion of moderate-to-severe aortic valve calcification (95.2% vs. 81.2%) (Table 1).
Baseline Patient Characteristics.*
| <80 (N = 69) | ≥80 (N = 21) | P-value | |
|---|---|---|---|
| Mean age (years) | 66.6 ± 5.1 (60–77) | 84.1 ± 3.0 (80–90) | <0.001 |
| Sex | 0.214 | ||
| Male | 34 (49.3%) | 14 (66.7%) | |
| Female | 35 (50.7%) | 7 (33.3%) | |
| BMI (kg/m2) | 22.7 ± 2.9 | 22.2 ± 3.1 | 0.488 |
| BSA (m2) | 1.55 ± 0.15 | 1.53 ± 0.15 | 0.512 |
| NYHA class III-IV | 62 (89.9%) | 16 (76.2%) | 0.141 |
| STS score (%) | 5.7 ± 1.0 | 6.1 ± 1.2 | 0.174 |
| Hypertension | 58 (84.1%) | 17 (81.0%) | 0.744 |
| Hyperlipidemia | 46 (66.7%) | 20 (95.2%) | 0.010 |
| Chronic heart failure | 18 (26.1%) | 9 (42.9%) | 0.176 |
| Diabetes mellitus | 20 (29.0%) | 5 (23.8%) | 0.784 |
| Prior myocardial infarction | 3 (4.3%) | 4 (19.0%) | 0.049 |
| Prior PCI | 7 (10.1%) | 10 (47.6%) | <0.001 |
| Prior coronary artery bypass graft | 0 (0.0%) | 0 (0.0%) | 1 |
| Cerebral vascular disease | 2 (2.9%) | 4 (19.0%) | 0.025 |
| Chronic atrial fibrillation | 5 (7.2%) | 4 (19.0%) | 0.205 |
| Chronic pulmonary disease | 7 (10.1%) | 9 (42.9%) | 0.002 |
| Chronic kidney disease | 10 (14.5%) | 4 (19.0%) | 0.732 |
| Chronic kidney dialysis | 1 (1.4%) | 0 (0.0%) | 1 |
| eGFR (mL/min/1.73 m2) | 67.6 ± 19.0 | 66.7 ± 18.0 | 0.843 |
| Prior permanent pacemaker | 1 (1.4%) | 0 (0.0%) | 1 |
| Echocardiographic findings | |||
| LVEF (%) | 60.4 ± 14.2 | 62.0 ± 15.7 | 0.692 |
| Aortic valve area (cm2) | 0.62 ± 0.18 | 0.63 ± 0.17 | 0.789 |
| Mean transaortic pressure gradient (mmHg) | 63.6 ± 18.8 | 65.0 ± 25.3 | 0.821 |
| Moderate/severe aortic regurgitation | 5 (7.2%) | 1 (4.8%) | 1 |
| Moderate/severe aortic calcification | 56 (81.2%) | 20 (95.2%) | 0.174 |
| MSCT findings | |||
| Type of aortic valve | 0.085 | ||
| TAV | 33 (49.3%) | 15 (71.4%) | |
| BAV | 34 (50.7%) | 6 (28.6%) | |
| Annulus diameter (mm) | 23.9 ± 2.9 | 23.5 ± 2.3 | 0.537 |
| Aortic angulation (degree) | 49.2 ± 9.8 | 49.0 ± 11.0 | 0.967 |
*Summary statistics are mean ± standard deviation or n (%).
BAV, bicuspid aortic valve; BMI, body mass index; eGFR, estimated glomerular filtration rate; LVEF, left ventricular ejection fraction; MSCT, multi-slice computed tomography; NYHA, New York Heart Association; PCI, percutaneous coronary intervention; STS, Society of Thoracic Surgeons; TAV, tricuspid aortic valve.
Procedural Characteristics and Outcomes
All patients in both age groups underwent TAVR in a hybrid room. Most patients received local anesthesia, and femoral artery access was used for valve implantation. Rapid ventricular pacing was achieved with a standard pacing wire in the right ventricle. The Evolut R/Pro self-expanding valve system (Medtronic, USA) with a 29 mm valve size was predominantly used. In the ≥80 year age group, one case (4.8%) of procedural mortality occurred, whereas this complication did not occur in the <80 year age group. Both groups had a comparable rate of major complications according to the VARC-2 criteria. The rate of successful valve implantation, on the basis of the VARC-2 criteria, was higher in the <80 year age group than the ≥80 year age group, but this difference was not statistically significant (97.1% vs. 90.5%, P = 0.231) (Table 2).
Procedural Characteristics and Outcomes.*
| <80 (N = 69) | ≥80 (N = 21) | P-value | |
|---|---|---|---|
| Hybrid catheterization laboratory | 69 (100.0%) | 21 (100.0%) | 1 |
| Valve-in-valve implantation | 2 (2.9%) | 0 (0.0%) | 1 |
| Type of anesthesia | 0.416 | ||
| General anesthesia | 20 (29.0%) | 4 (19.0%) | |
| Local anesthesia | 49 (71.0%) | 17 (81.0%) | |
| Type of temporary ventricular rapid pacing | 0.725 | ||
| Rapid pacing via classic right ventricle | 58 (84.1%) | 19 (90.5%) | |
| Rapid pacing via left ventricular guidewire | 11 (15.9%) | 2 (9.5%) | |
| Type of TAV | 1 | ||
| Self-expandable system Evolut R/Pro | 66 (95.7%) | 21 (100.0%) | |
| Self-expandable system Portico | 2 (2.9%) | 0 (0.0%) | |
| Balloon-expandable system Sapien 3 | 1 (1.4%) | 0 (0.0%) | |
| Type of access route | 0.554 | ||
| Transfemoral | 67 (97.1%) | 20 (95.2%) | |
| Trans-subclavian | 1 (1.4%) | 1 (4.8%) | |
| Transcarotid | 1 (1.4%) | 0 (0.0%) | |
| Others | 0 (0.0%) | 0 (0.0%) | |
| Valve size (mm) | 0.241 | ||
| 29 | 33 (47.8%) | 10 (47.6%) | |
| 26 | 12 (17.4%) | 8 (38.1%) | |
| 34 | 13 (18.8%) | 3 (14.3%) | |
| 23 | 9 (13.0%) | 0 (0.0%) | |
| 25 | 1 (1.4%) | 0 (0.0%) | |
| 27 | 1 (1.4%) | 0 (0.0%) | |
| Mortality | 0 (0.0%) | 1 (4.8%) | 0.233 |
| Disabling stroke | 1 (1.4%) | 0 (0.0%) | 1 |
| Life-threatening bleeding | 1 (1.4%) | 1 (4.8%) | 0.414 |
| Major vascular complication | 2 (2.8%) | 1 (4.8%) | 0.554 |
| Coronary artery obstruction requiring intervention | 0 (0.0%) | 1 (4.8%) | 0.233 |
| Annulus rupture or ventricular septal perforation | 0 (0.0%) | 0 (0.0%) | 1 |
| Valve malpositioning | 2 (2.8%) | 0 (0.0%) | 1 |
| Complete atrioventricular block | 5 (7.2%) | 1 (4.8%) | 1 |
| Conversion to open heart surgery | 1 (1.4%) | 2 (9.5%) | 0.135 |
| Conversion to SAVR | 1 (1.4%) | 1 (4.8%) | 0.414 |
| Moderate to severe paravalvular leak | 1 (1.5%) | 0 (0.0%) | 1 |
| Implantation of two valves | 2 (2.8%) | 0 (0.0%) | 1 |
| Device success | 67 (97.1%) | 19 (90.5%) | 0.231 |
*Summary statistics are mean ± standard deviation or n (%).
SAVR, surgical aortic valve replacement; TAV, tricuspid aortic valve.
30-Day and 1-Year Outcomes
The clinical outcomes in both patient groups at 30 days and 1 year after TAVR are presented in Table 3. The mortality rate from all causes at 30 days (5.0% vs. 1.5%, P = 0.405) and 1 year (11.8% vs. 3.7%, P = 0.241) was higher in the ≥80 year age group than the <80 year age group, but these differences were not statistically significant. Figure 1 illustrates the survival rate between patient groups at 1 year after TAVI. The rates of other clinical outcomes, according to VARC-2, used to assess early safety at 30 days and clinical effectiveness at 1 year after TAVR also did not significantly differ between age groups. All surviving patients in each age group at the 30-day and 1-year time points underwent assessment of LVEF, mean transaortic pressure gradient, and NYHA functional class; these assessments were performed on 67 and 52 patients, respectively, in the <80 year age group, and on 19 and 15 patients, respectively, in the ≥80 year age group. LVEF showed significant improvements in both patient groups at 30 days and 1 year, as compared with pre-TAVR; however, the differences in LVEF between patient groups at these time points were not statistically significant (Figure 2A). The mean transaortic pressure gradient decreased sharply immediately after valve implantation in both patient groups, and this gradient decrease was significant at discharge, 30 days, and 1 year, with respect to pre-TAVR. Comparison of the changes in mean transaortic pressure gradient between age groups at each follow-up time point indicated no statistically significant differences (Figure 2B). At the 30 day and 1-year follow-up, except for the deceased patients, no cases of NYHA class III-IV cases remained in either patient group (Figure 2C).

Kaplan-Meier Survival Curve for 1-Year All-Cause Mortality after TAVI.
TAVI, transcatheter aortic valve implantation.
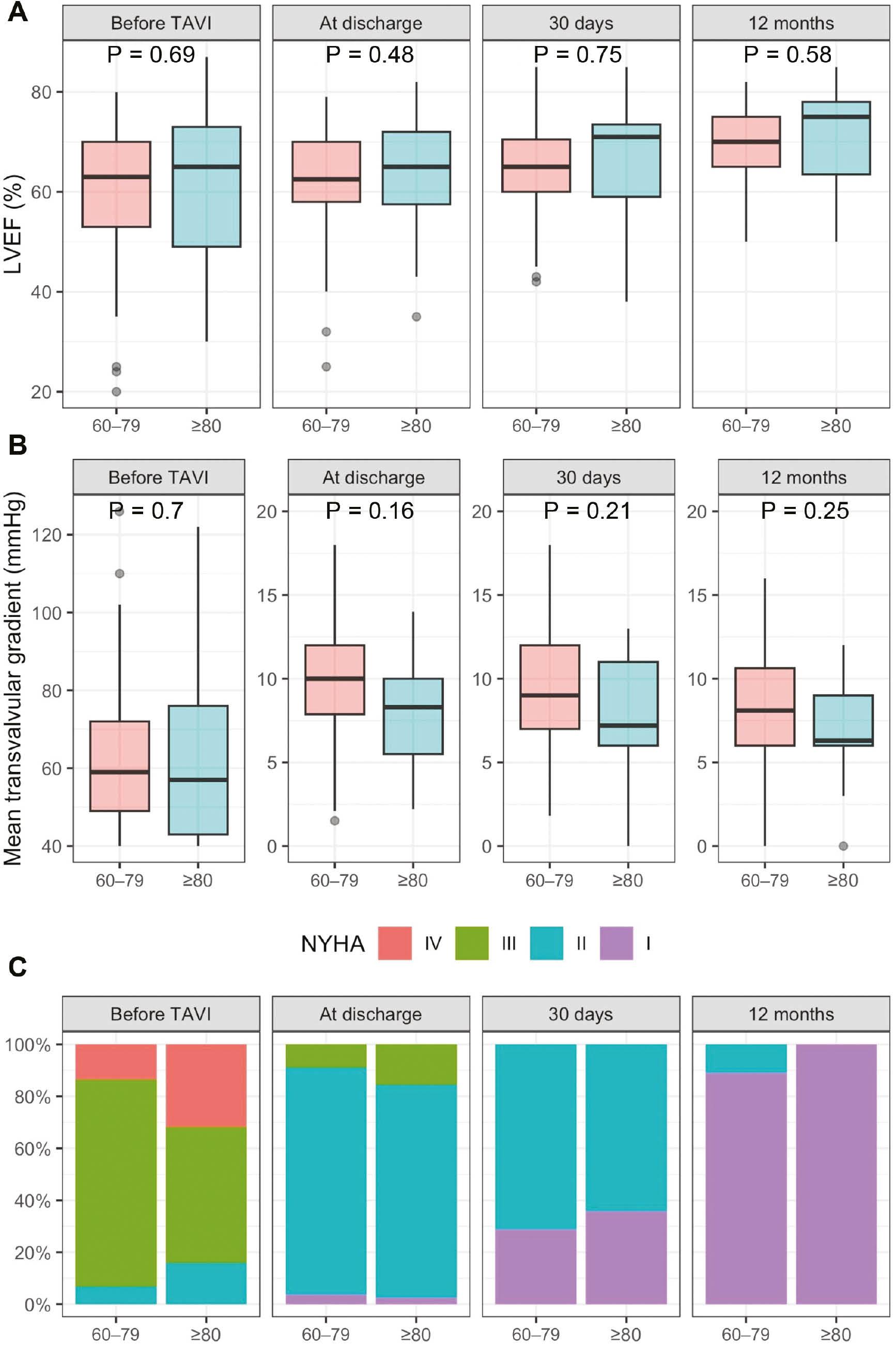
LVEF, mean Transvalvular Gradient and NYHA before and after TAVI.
(A) Changes in LVEF before TAVI and at discharge, 30 days, and 12 months. (B) Changes in mean transvalvular gradient before TAVI and at discharge, 30 days, and 12 months. (C) Changes in NYHA before TAVI and at discharge, 30 days, and 12 months. LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; TAVI, transcatheter aortic valve implantation.
30-Day and 1-Year Outcomes.*
| <80 | ≥80 | P-value | |
|---|---|---|---|
| 30-day outcomes | N = 68 | N = 20 | |
| All-cause mortality | 1 (1.5%) | 1 (5.0%) | 0.405 |
| Cardiovascular mortality | 1 (1.5%) | 1 (5.0%) | 0.405 |
| Disabling stroke | 2 (3.0%) | 0 (0.0%) | 1 |
| Major vascular complication | 2 (2.9%) | 1 (5.0%) | 0.543 |
| Life-threatening bleeding | 1 (1.5%) | 1 (5.0%) | 0.405 |
| Stage 2 or 3 acute kidney injury | 0 (0.0%) | 0 (0.0%) | 1 |
| Valve-related dysfunction requiring repeat procedure (BAV, TAVI, or SAVR) | 0 (0.0%) | 0 (0.0%) | 1 |
| Coronary artery obstruction requiring intervention | 0 (0.0%) | 1 (5.0%) | 0.227 |
| New pacemaker implantation | 5 (7.4%) | 2 (10.0%) | 0.655 |
| Moderate/severe paravalvular leak | 2 (3.0%) | 0 (0.0%) | 1 |
| 1-year outcomes | N = 54 | N = 17 | |
| All-cause mortality | 2 (3.7%) | 2 (11.8%) | 0.241 |
| Cardiovascular mortality | 2 (3.7%) | 2 (11.8%) | 0.241 |
| Disabling stroke | 2 (3.7%) | 0 (0.0%) | 1 |
| Requiring hospitalizations for valve-related symptoms or worsening heart failure | 2 (3.7%) | 0 (0.0%) | 1 |
| NYHA class | 1 | ||
| I | 49 (94.2%) | 15 (100.0%) | |
| II | 3 (5.8%) | 0 (0.0%) | |
| III or IV | 0 (0.0%) | 0 (0.0%) | |
| Valve-related disfunction | 0 (0.0) | 0 (0.0) | 1 |
| New pacemaker implantation | 5 (9.3%) | 2 (11.8%) | 0.670 |
| Moderate/severe paravalvular leak | 2 (3.7%) | 0 (0.0%) | 1 |
| Prosthetic valve endocarditis or thrombosis | 0 (0.0) | 0 (0.0) | 1 |
*Summary statistics are mean ± standard deviation or n (%).
BAV, bicuspid aortic valve; SAVR, surgical aortic valve replacement; TAVI, transcatheter aortic valve implantation.
Discussion
The results from the first study on Vietnamese patients with severe AS at moderate surgical risk, including 21 patients ≥80 years old and 69 patients <80 years old (60–79 years), who underwent TAVR at a single center, demonstrated that the very old patients often had more comorbidities. However, the primary clinical outcomes according to VARC-2 criteria during the procedure, at 30 days, and at 1 year were similar between age groups.
The two widely used surgical risk scores in TAVR, the STS score and EuroSCORE II, incorporate age as a factor, and surgical risk increases with advancing age [21]. However, the effects of age on clinical outcomes vary among Western studies [17]. In an analysis evaluating the influence of age on TAVR outcomes based on data from the Swiss TAVI Registry, which included 7097 patients divided into four age groups: <70 years (n = 324, mean age 64.6 ± 5.8 and STS score 3.5 ± 4.1), 70–79 years (n = 1913, mean age 76.5 ± 2.6 and STS score 4.0 ± 3.7), 80–89 years (n = 4353, mean age 84.5 ± 2.7 and STS score 5.6 ± 4.0), and ≥90 years (n=507, mean age 92.0 ± 1.7 and STS score 8.2 ± 4.7), all-cause mortality, stroke, and permanent pacemaker implantation significantly increased with age (all P < 0.05), whereas other major outcomes according to VARC-2 showed no differences. However, other observational studies comparing the clinical outcomes of patients ≥85 years (or 80 years) old with younger patient groups have not found an influence of age on the rates of all-cause mortality at 30 days and 1 year [13]. In an observational study by van der Kley et al. in the Dutch population, including 105 patients ≤80 years old (mean age 74.8 ± 5.5 and EuroSCORE I 21.2% ± 14.8%) and 135 patients >80 years old (mean age 85.8 ± 3.1 and EuroSCORE I 24.6% ± 14.1%) with severe aortic stenosis undergoing TAVR, no significant difference in all-cause mortality was found at 30 days (9.5% vs. 7.4%, P = 0.557) and 1 year (20.9% vs. 15.6%, P = 0.276) between age groups [14]. In another analysis of patients with severe aortic stenosis undergoing TAVR in Poland, including 200 patients ≥85 years old (mean age 87.4 and EuroSCORE II 7.2) and 417 patients <80 years old (mean age 76.8 and EuroSCORE II 6.5), no significant difference in all-cause mortality was observed between age groups at 30 days (5.5% vs. 4.3%, P = 0.51), 1 year (17.9% vs. 12.8%, P = 0.06), 2 years (25.9% vs. 19.8%, P = 0.13), and 5 years (49.3% vs. 45.1%, P = 0.51) [16]. Moreover, age did not significantly affect TAVR clinical outcomes at 30 days in a study by Ofer et al. in the Israeli population, comparing patients ≤85 years old (mean age 80.5 ± 4.0 and EuroSCORE 26.3 ± 13) or >85 years old (mean age 88.8 ± 2.5 and EuroSCORE 24.0 ± 14.5) with high surgical risk undergoing TAVR [15].
Our study on 21 patients ≥80 years old (mean age 84.1 ± 3.0 and STS score 6.1 ± 1.2) and 69 patients <80 years old (mean age 66.6 ± 5.1 and STS score 5.7 ± 1.0) with severe AS undergoing TAVR at a center serving the Vietnamese population also showed no significant difference in all-cause mortality at 30 days (5.0% vs. 1.5%, P = 0.405) and 1 year (11.8% vs. 3.7%, P = 0.241) between age groups. The rates of other clinical outcomes, according to VARC-2, at different follow-up time points were also not statistically significant. One notable difference between our study and others analyzing the effects of age on TAVR clinical outcomes was that the average age in our younger patient group was relatively younger (66.6 ± 5.1), and the proportion of BAV was quite high in both analyzed groups. BAV has been entirely excluded in RCTs of TAVI, and in the real world, TAVR indications for this patient group are also limited because of anatomical characteristics unfavorable for TAVR procedures [22, 23]. The rate of BAV in our study was relatively high with respect to those in studies in other populations, except for China [19]. However, this unfavorable characteristic did not significantly affect the clinical outcomes, including the success rate of valve implantation, when TAVR was performed in patients ≥80 years old and younger patients. Furthermore, our study also demonstrated improvements in LVEF, the mean pressure gradient across the valve, and NYHA classification at follow-up time points after TAVR compared with pre-TAVR, and no statistically significant differences in these changes were observed between age groups. These results have not been frequently observed in other studies analyzing the effects of age on TAVR outcomes.
A major limitation of our study is its observational nature; its small patient sample; and an approximately 1:3 proportion of patients ≥80 years old to patients <80 years old at follow-up time points, which might have led to bias in comparisons of outcomes between age groups, and between this study and other studies. Additionally, the effects of frailty, a common geriatric syndrome prevalent in older people and known to have adverse effects on the outcomes of patients undergoing aortic valve intervention, was not documented or analyzed in this study.
Conclusion
The results of this study on 21 patients ≥80 years old and 69 patients <80 years old with symptomatic severe AS undergoing TAVR with moderate surgical risk at a center in Vietnam showed that, compared with the younger patient group, the ≥80 year old group had more comorbidities. However, the primary clinical outcomes, according to VARC-2 criteria, during the procedure, at 30 days, and at 1 year did not significantly differ between groups. Nevertheless, more extensive investigations involving larger patient cohorts are essential for more comprehensive understanding of age-associated effects on TAVR outcomes in patients with similar characteristics.
