Introduction
Breast reduction surgery is one of the most commonly performed cosmetic procedures.(1) It is a life changing procedure for many women in both physical and psychological aspects.(1)
Reducing the size and weight in bilateral breast reduction is not enough. Currently, the goal is to also achieve a pleasing shape and similar looking breasts post reduction.(2) Another important goal is to preserve function, sensation and an ideal nipple areola complex (NAC) position.(1,3) Regardless of the reduction technique used in reduction mammoplasty, the proper position, size, and shape of the NAC is challenging.(2,4)
In plastic surgery the main aim of bilateral breast reduction is to obtain an as natural appearance as possible and to meet the patient's expectations and satisfaction.(4)
The breast optimal size is calculated in proportions of upper to lower pole breast size, which is 1:3, and the widely accepted standard for areola diameter is 38–45 mm.(4–6) In addition, the position of the NAC has a significant impact on the overall appearance of the breast.(3) The NAC is a very critical landmark affecting the final aesthetic result.(7)
The ideal new NAC should be:
The postoperative long-term result is of great importance in the overall long-term aesthetic result.(4)Patients and Methods
In this study, we aimed to review the immediate and long-term results after using the superomedial (or superior-medial) pedicle technique (SMP), in terms of NAC position, and patient satisfaction with the new NAC in a one-year follow-up. Using the SMP allows large volume resection and wide transposition of the NAC. The base of the pedicle is designed to extend superior and lateral to the breast meridian, to include the descending branches from the second intercostal space with the internal mammary perforators from the third and fourth intercostal space.
Unfortunately, the spread of the Covid-19 pandemic resulted in new hospital regulations and precautions, so that no elective surgery was allowed which, in turn, had a huge impact on the number of patients being recruited for the study. Furthermore, many patients experienced financial insecurity due to job losses and the overall economic collapse. Patients were no longer able to pay the surgery fees as the elective breast reduction procedure is not free of charge. This limitation impacted hugely on our study resulting in the small sample size.
Methodology
Study Design
This was a one week, one month and one-year prospective observational study of NAC position post breast reduction surgery, conducted at the Helen Joseph Academic Hospital on adult female patients. The three and six month evaluations were eliminated because of the Covid-19 pandemic with strict hospital lockdown regulations and for patient safety.
Patients satisfaction with the end result of the new NAC were assessed using a questionnaire at the one year follow-up by the primary investigator in the absence of any surgeons, to eliminate the risk of bias. Written consent was obtained from all patients prior to participation in the study. Study clearance from the institutional review committee of Helen Joseph Hospital and ethics clearance from the University of the Witwatersrand Human Research Ethics Committee (Medical) with certificate number M190967, were obtained.
Inclusion criteria
All adult female patients over the age of 18 years, who had breast reduction surgery using a Wise pattern skin excision with the SMP technique, including cosmetic and oncoplastic breast reduction with SMP were included in the study.
Exclusion criteria
Pregnancy post reduction in the one-year follow-up period of this study. Only one patient was excluded from this study as she got pregnant in the postoperative period.
Between February 2020 and June 2021, 11 patients comprising 19 breasts were included in this study (three of the eight patients had unilateral breast reductions as mastectomy was done on the cancer site). The mean and median age of these patients was 36.8 and 35.0 years, respectively (range: 21–65 years) and the mean and median BMI +++++++was 29.8 kg/m2 and 28.7 kg/m2 (range: 22.7 to 37 kg/m2), respectively.
Patient demographics recording age, race, smoking history, alcohol, drugs, contraceptive usage, comorbidity, retrovirus disease (RVD) status were recorded.
Of the 11 patients in the study group, the majority (72.7%, 8/11) were between 20 and 39 years of age. Only two patients were in the 40–49 year category and one patient was older than 60 years. The race distribution of patients in this study was 63.6% black, 27.7% coloured and 9.1% white. The 27.3% (3/11) of patients with comorbidities were all known hypertensives on medical treatment. Only one patient (9.1%) of the study group was RVD positive and on anti-retroviral (ARV).
In this study, 27.3% (3/11) of the study group had elective bilateral breast reductions as all three were suffering from symptoms of large breast. The majority 72.7% (8/11) of patients had oncoplastic breast reduction, with wide local excision of the cancer site breast and symmetrisation procedure on the contralateral side, using the SMP for both.
The technique preformed for all patients was the SMP with the Wise pattern skin excision. Residents in different stages of their training performed the procedures and were all supervised by the same specialist surgeon (AR). All the measurements were recorded by the principal investigator (AA) as follows: nipple to inferior mammary fold (IMF), sternal notch to the nipple (SNTN) and NAC diameter. The new NAC position was decided by the surgeon during the preoperative marking, using the well-known Pitanguy point method as described by Pitanguy,(10) which uses the IMF as reference. All measurements were recorded preoperatively, at one week, one month and one year postoperatively. Measurements were recorded at each clinic visit. All patients were advised to continue wearing a supportive sport bra to reduce the risk of inferior migration of the breast parenchyma resulting in superior displacement of the NAC, with respect to the breast mound, known as bottoming out.
Results
By using the Wise-pattern skin excision with SMP technique, we had no complications related to wound healing, the NAC, hematoma, seroma or infection. Drainage was used in all patients. The average total reduction per breast was 661.8 g (range: 155.0–1505.0 g). The average and range of patient measurements including SNTN, nipple to IMF and NAC diameter, were recorded preoperatively, then postoperatively at one week, one month and one year follow-up as shown in Table 1.
All measurements of all breasts.
| Measurements | Average (Range), (cm) |
|---|---|
| Preoperative : SN to Nipple | 21.7 (19–24) |
| One week: SN to Nipple | 21.7 (19–24) |
| One month: SN to Nipple | 22.1 (20–24) |
| One year: SN to Nipple | 23.5 (20–26) |
| Preoperative: Nipple to IMF | 5.8 (5–6) |
| One week: Nipple to IMF | 5.8 (5–6) |
| One month: Nipple to IMF | 6.4 (5–8) |
| One year: Nipple to IMF | 9.3 (6–16) |
| Preoperative : Areolar diameter | 3.6 (3–4.5) |
| One week: Areolar diameter | 3.6 (3–4.5) |
| One month: Areolar diameter | 3.7 (3–5) |
| One year: Areolar diameter | 4.3 (3.5–5) |
SN, sternal notch; IMF, inframammary fold.
There were no changes in any of the measurements at one week post reduction. The average differences in nipple position to sternal notch were inferior transposition by 0.32 cm and 1.74 cm at one month and one year, respectively, compared to the preoperative measurements. The nipple position at one year was located on average 1.74 cm lower (range: 1.00–3.00 cm). These changes were statistically significant at one week and one year (p=0.014 and p<0.0001), respectively. The majority of changes in nipple position to sternal notch were noticed in the one year follow-up post reduction as shown in Figures 1 and 2.
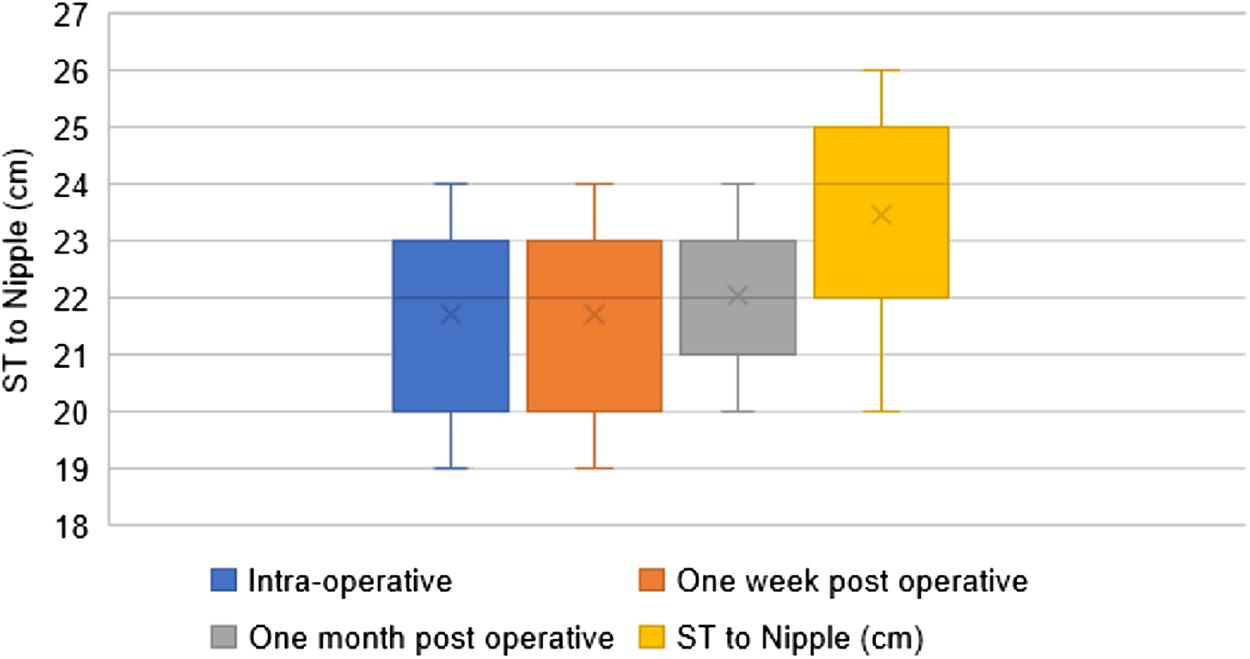
Changes in sternal notch to nipple position, comparing intra-operative measurements (blue), to one week (orange), one month (grey) and one year (yellow) follow-up. The horizontal lines inside the boxes represent the median, while the X represents the mean.
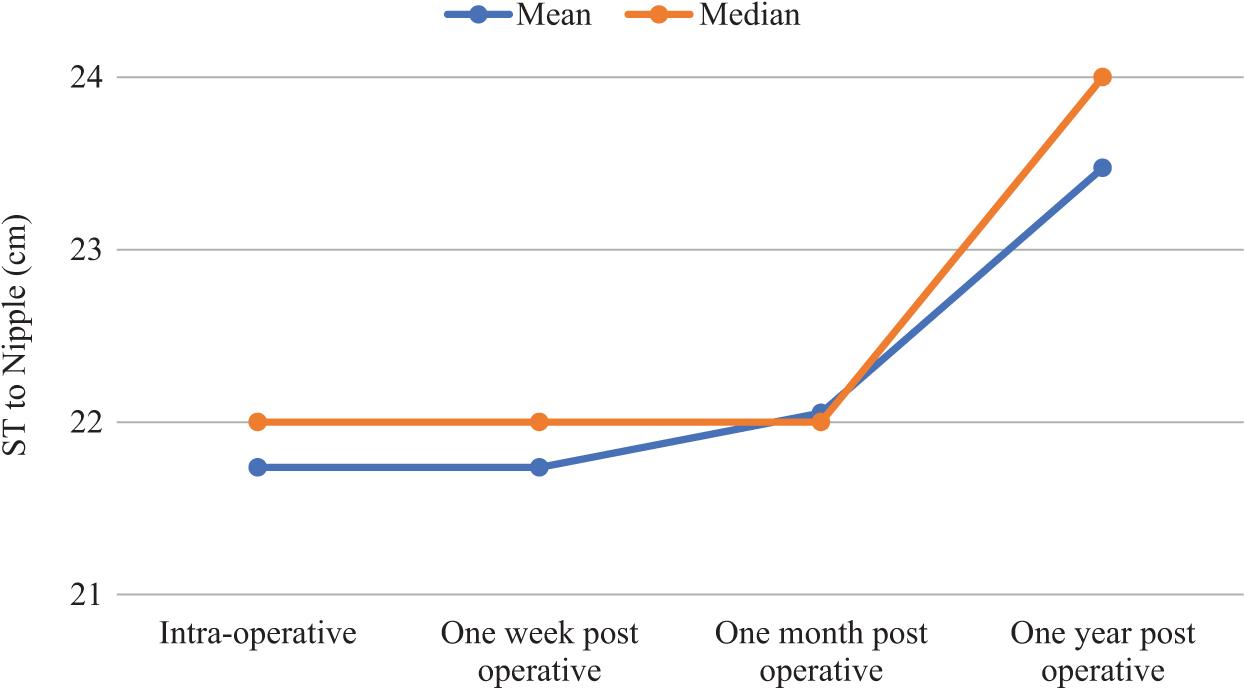
Changes of nipple position to sternal notch over one year period. Vertical axis is distance in (cm). The blue line represents the mean and the orange/red line the median. indicating the changes in the period between one month and one year.
No changes were noticed in the distance between the nipples and IMFs at one week, while these distances started to increase noticeably at one month and major increases were noticed at the one year follow-up. Both the one month and one year changes were statistically significant with p-values <0.01 and 0.0001 respectively. The average change in one year was 9.32 cm (range: 6.00–16.0 cm). The mean increase in the distance was 0.61 cm at one month and 3.53 cm at one year, compared to the preoperative measurements. Figures 3 and 4, demonstrate the changes in one week, one month and one year follow-up post reduction. The curve in Figure 4 shows that the biggest increase in distance occurred between one month and one year.
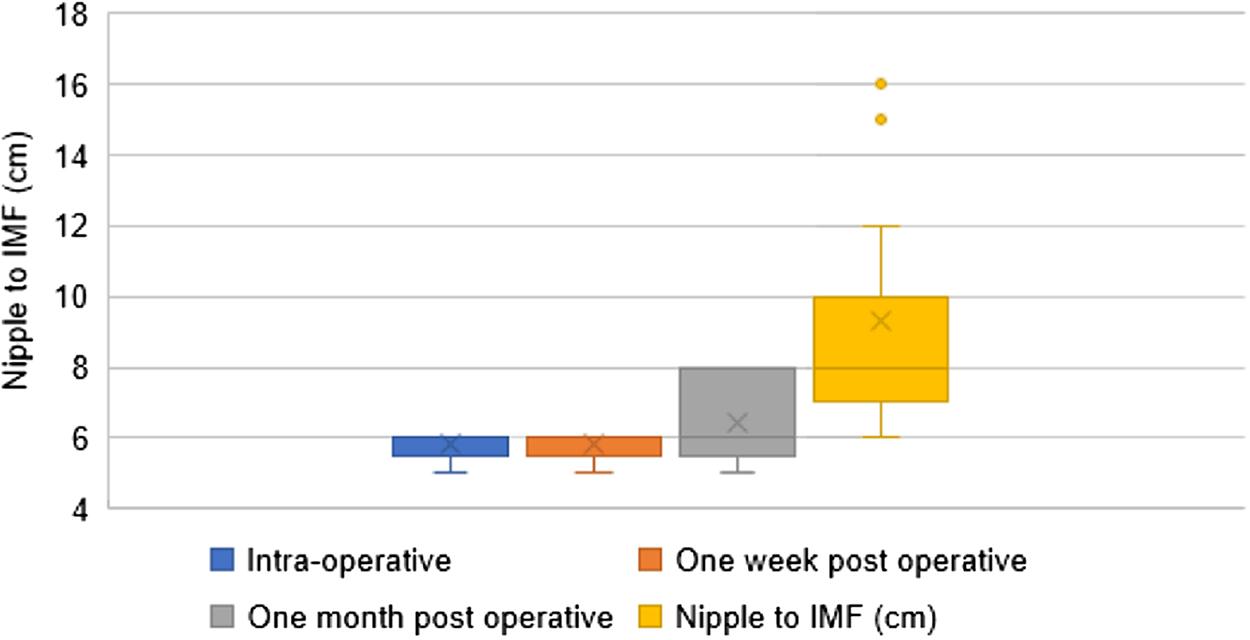
Changes in nipple to IMF distance over the postoperative period. The line inside the boxes represents the median, while the X represents the mean.
An increase in the nipple to IMF distance was noticed at one month and especially at one year. Only one patient with bilateral breast reduction fell outside the whisker plot graph as shown in Figure 3 at one year. After reviewing this patient's information, the only factor that was different from all other patients was a marked increase in BMI as an 11 kg increase in body weight was recorded.
The areola diameter increased over one year with an average of 0.67 cm (range: 0.2–1.2 cm) compared to preoperative measurements (Figure 5), which was statistically significant (p < 0.00015).
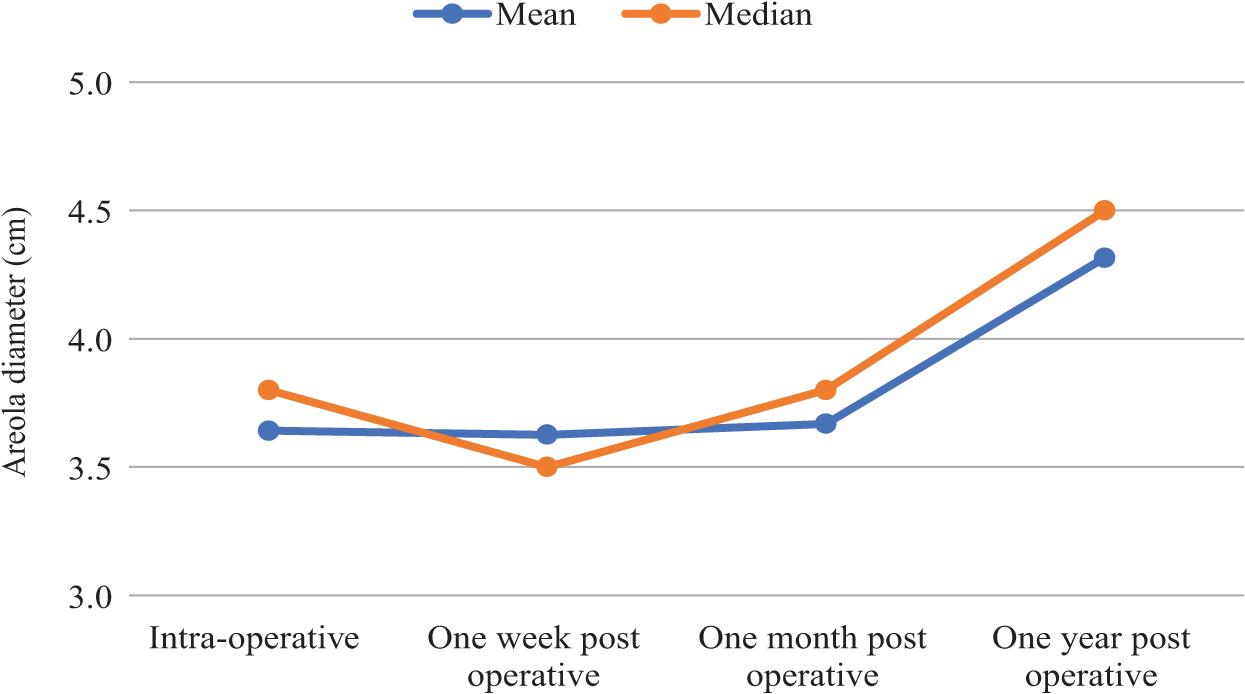
The average areola diameter changes from intra-operative to one week, one month and one year.
With the measurements recorded at one week, one month and one year postoperatively, the most significant statistical changes were observed at one year compared to the intra-operative measurements as summarized in Table 2.
Comparison of intra-operative measurements to one year follow-up measurements for all breasts.
| Measurements | Average (Range), cm | p |
|---|---|---|
| SN to N | 1.47 (1–3) | <0.00009* |
| N to IMF | 3.35 (1–10) | <0.00012* |
| Areolar diameter | 0.67 (0–1.2) | <0.00015* |
SN, sternal notch; N, nipple; IMF, inframammary fold.
*Statistically significant.
Patient satisfaction with their NAC was evaluated at the one year follow-up visit, using a questionnaire. The questions were related to nipple position, shape, pigmentation, projection, sensation, size, overall symmetry and the overall breast reduction result. The last two questions were whether the patient would have the procedure done again and whether they would recommend the procedure to friends. All study patients answered the questionnaire. The vast majority (90%) of patients had completely normal sensation from week one, only one patient who had both breasts reduced did not have full sensory recovery even at the one year follow-up visit. Regarding the breast size and shape, 82% of patients were satisfied, while only 18% thought the breasts were still a bit large. All patients (100%) were satisfied with the colour of the nipples with no hypo- or hyper-pigmentation, while 90% were satisfied with the nipple position. Only one patient was not pleased with the nipple projection, while the other 90% were satisfied. Overall 90% of the patients were satisfied with the end result.
Discussion
There are several studies in the literature that investigated the long term result of nipple position post reduction mammoplasty with different pedicles and various skin excisions with each technique showing different results. Each technique has different advantages and disadvantages, without any technique described as superior to another.
Reus and Mathes(11) reviewed 22 patients over 4.2 years in whom the inferior pedicle and inverted T skin incision technique was used, and found that there were no changes in midclavicular to nipple distance. However, the vertical scar increased over time from inferior migration of the breast parenchyma resulting in superior displacement of the NAC with respect to the breast mound (known as bottoming out). They found an average 72% lengthening in the vertical limb scar with resection weights greater than 1200 g, versus 48% scar lengthening in resections of between 500 and 1200 g.(11)
In 2002, Erdogan et al.(12) documented similar findings five years after surgery on 52 patients using the inferior pedicle technique. This study showed that the vertical limb scar increased in length by 49% with resection weights of between 500 and 1200 g.
In concurrence, Abramson et al.(13) presented a series of 88 patients who underwent breast reductions using the medial pedicle with a Wise pattern skin resection. The nipple to IMF distance increased on average by 34% for reduction weights greater than 1200 g and the mean increase in distance was 9.4 cm at one year.
Kemaloğlu and Özocak(14) compared the inferior pedicle with the SMP reduction using the Wise pattern skin excision, and found that the average lengthening of the NAC to IMF was 2.08 cm for the inferior pedicle and it increased to 2.20 cm with the SMP pedicle.
The fate of the nipple and the inferior pole length in vertical scar reduction mammoplasty was studied by Ahmad and Lista.(15) They reported that the NAC was 1 cm higher and the distance between the IMF and inferior border of the NAC were shorter at a four year follow-up.
Keck et al.(16) investigated the postoperative changes after vertical mammoplasty at one year, and reported that the main changes took place in the first three months after surgery. The average increase in the nipple diameter was 28% after surgery, and the average increase in notch to nipple distance was 17%.
In this study we used a Wise pattern key hole skin incision with a SMP pedicle. Importantly, the SMP pedicle has a good blood supply to the NAC and preserves sensation. Indeed, patients reported good and quick sensory recovery. The aim of this prospective observational study was to address and measure the changes related to NAC position postoperatively compared to preoperatively. This technique is safe with no complications related to NAC specifically, or to the breast in general.
We found that the notch to nipple measurement increased by 6% (1.74 cm) and the nipple to IMF distance increased by 46% (3.53 cm) with a resection weight up to 1500 g, compared to Kemaloğlu and Özocak(14) results, which were 2.20 cm with an average resection of 1 345 g. The areola diameter in our study stretched out by 18% at one year.
Conclusions
The results of this breast reduction surgery study using the superomedial pedicle technique, provide objective measurements at one year observation of nipple position related to notch, IMF, and NAC diameter with a high degree of satisfaction. Importantly, there were no early or late complications relating to the NAC specifically or to wound healing in general, using a wise pattern skin excision. Remarkably, 90% of the patients were satisfied with the end result of the new NAC and 90% had no changes on fine touch sensation post reduction.

