Introduction
A coupling medium is used in ultrasonography to improve the sound wave conduction between the instrument probe and the patient's tissue. (1) Ultrasound gel is the gold standard coupling medium, commonly used in various diagnostic medical fields such as obstetrics, cardiology and urology. (2) However, since ultrasound gel is often out of stock in rural hospitals due to its frequent use, suppliers’ inaccessibility to remote locations and due to hospital financial constraints, the researchers aimed to find an adequate but cheaper, more readily available alternative. Therefore, the authors proposed using cheaper petroleum jelly (Vaseline, Blue Seal Original), which is viscous, melts at body temperature, causes no friction, is non-allergenic, non-irritant (3) and is easily wiped off the skin surface, as an alternative to conventional renal ultrasound gel. Currently there is no literature regarding the use of petroleum jelly to perform renal ultrasound imaging. Thus the aim of the study was to determine if cost saving petroleum jelly ultrasound kidney imaging is adequate for clinical use.
Materials and Methods
This was a prospective study conducted at Thelle Mogoerane Regional Hospital (TMRH) in the East Rand of Johannesburg, South Africa. Study patients presenting to the TMRH Urology Department were consecutively enrolled in the sequence of their presentation, regardless of gender, weight, or BMI, for a routine renal ultrasound of the left kidney. Images were obtained with both ultrasound gel as well as petroleum jelly in each patient. Patients with wound or skin conditions affecting the abdominal- or flank area, were excluded from the study. The study included 42 patients aged between 20 and 75 years. All patients consented to partake anonymously in the study.
A single ultrasonographer using a Philips Clear Vue 550 ultrasound instrument with a C5-2 broadband curved array probe with a frequency range of 2–5 MHz, scored each image from 1–3 (1 worst; 3 best) with regard to the following criteria:(4)
- 1.
Penetration: Demonstration of the kidney at increasing depth.
- 2.
Detail: Sharpness of the outline of the solid and fluid filled areas.
- 3.
Total image quality: Contrast between solid and fluid areas and absence of artifact or noise.
The ultrasonographer also commented on whether the imaging was adequate for clinical use (yes/no) and which one of the two images’ quality was better. In addition, in order to minimise subjective evaluation and possible bias of a single ultrasonographer, 40 doctors of two independent Urology and Radiology Departments completed a blinded questionnaire, determining which image of each pair of 42 images was adequate for clinical use. The Human Research Ethics Committee of the University of the Witwatersrand approved the study.
Data were analysed using Stata Version 14.2. Numerical and categorical values were statistically analysed, while inferential statistics were applied to the three parameters scored out of 3, using the paired T-test. A confidence interval of 95% and a p value of < 0.05 indicated statistical significance.
Results
Ultrasonographer Assessment:
Ultrasound gel produced images that were adequate for clinical use more often than petroleum jelly: 95.25% (n=40/42) vs 88.10% (n=37/42) as shown in Figure 1.
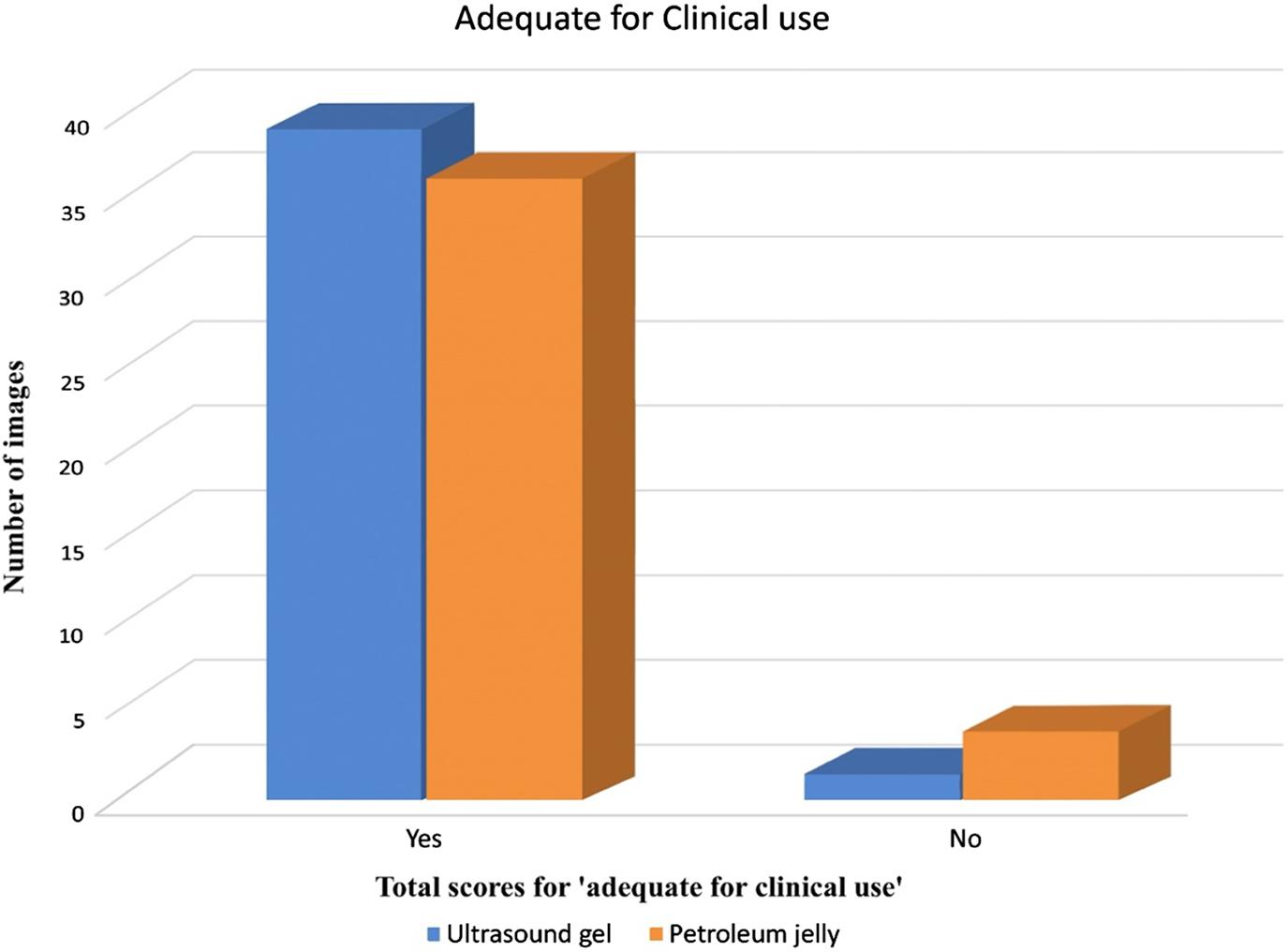
Total scores for ‘adequate for clinical use’ parameter for ultrasound gel and petroleum jelly images
Ultrasound gel vs petroleum jelly for each respective parameter: Penetration 83.33% (n=35/42) vs 61.90% (n=26/42), detail 71.43% (n=30/42) vs 45.24% (n=19/42) and total image quality 76.19% (n=32/42) vs 61.90% (n=26/42). The mean scores for each parameter are shown in Figure 2.
Overall the best imaging was most often obtained in 61.9% (n=26/42) of patients using ultrasound gel. However, petroleum jelly produced better imaging in 28.57% (n=12/42) of patients. The image quality was seldom equal (9.52%, n=4/42).
Regarding penetration, the ultrasound gel scored 2.81 0.45 compared to petroleum jelly 2.57 0.59 with a statistically significant higher mean score for ultrasound gel of 0.238 (95% CI, 0.034 to 0.442) (p=0.024).
With regard to image detail, the ultrasound gel scored 2.62 0.66 compared to petroleum jelly 2.360.66 with a statistically significant higher mean score for ultrasound gel of 0.2619 (95% CI, 0.023 to 0.501) (p=0.0325).
For the ultrasound total image quality, the ultrasound gel scored 2.740.50 compared to petroleum jelly 2.52 0.67 with a statistically significant higher mean score of 0.2143 (95% CI, 0.0254 to 0.4032) (p=0.0272) for the ultrasound gel.
Doctors’ Assessment
Forty doctors from the Urology (n=29) and Radiology Departments (n=11) of two universities reviewed the 42 patients’ left kidney ultrasound gel and petroleum jelly images (84 images in total) using a blinded questionnaire (Table 1). The doctors found that 16/42 (38.1%) images using petroleum jelly were best for clinical use, compared with 24/42 (57.1%) using ultrasound gel, while 2/42 (4.8%) images were rated equal.
Discussion
Overall both the sonographer and doctors’ assessment found better images with ultrasound gel (61.9% vs 57.1%). However, petroleum jelly performed better in the doctor's assessments compared to the sonographer's assessment of the images (40% vs 26%).
Ultrasound gel images adequate for clinical use was found in 95% of patients and in 88% of patients where images were obtained with petroleum jelly. Ultrasound gel had statistically significant better mean scores than petroleum jelly in all categories of image acquisition i.e. penetration, detail and total image quality. Thus, although ultrasound gel use overall had better image quality, adequate image acquisition with petroleum jelly was found in almost 90% of patients.
The average total cost of petroleum jelly and one tongue depressor was 42c per patient opposed to an average of 60c for ultrasound gel (Brunel Laboratoria), totalling a cost saving of 30% per renal ultrasound image with petroleum jelly.
Limitations
The sample size of this study was relatively small and thus the significant differences in image quality obtained with petroleum jelly and ultrasound gel may to some extent be attributable to the small sample size.
Conclusions
Although ultrasound gel remains the gold standard coupling medium for ultrasound, in the setting where ultrasound gel is not available, petroleum jelly is a good affordable alternative to obtain clinically satisfactory renal ultrasound imaging. If an alternative dispensing method for petroleum jelly can be found: single sachets or a squeezable nozzle dispensing bottle, a further reduction in cost per patient could be achieved. These study findings are important to all countries where medical resources are limited, and to hospitals/clinics situated in remote areas who may not have timeous access to ultrasound gel.


