INTRODUCTION
Cerebral palsy (CP) is a nonprogressive neurological disorder that affects motor function and coordination and leads to deterioration in function. This disorder affects the developing brain during fetal life or at infancy up to 2 years of age. The most common type of CP is the unilateral type (Emara et al., 2022).
According to recent systematic review, the recent World Wide prevalence of CP was 1.6 per 1000 births (McIntyre et al., 2022). A slightly higher prevalence rate (1.8/1000 live births) was reported in Arabic-speaking countries including Saudi Arabia, Egypt, and Jordan (Mushta et al., 2022).
Among children with CP, spasticity is a common problem characterized by increased muscle tone, stiffness, and involuntary muscle contractions. It can make it challenging to walk, sit, or even hold objects. It can also cause pain and discomfort, as well as increase the risk of developing other musculoskeletal problems such as contractures and deformities (Ayvat et al., 2021).
There are various treatment options available to manage spasticity in children with CP. These options include physical therapy, occupational therapy, medication, and surgery. One emerging treatment modality is body vibration.
Vibration is the mechanical stimulus characterized by oscillatory movements. Vibration can be applied locally or throughout the body, when applied to the whole body it is referred to as whole-body vibration (WBV). This method of treatment has been incorporated and frequently used in the field of physical therapy and rehabilitation (Tekin and Kavlak, 2021). WBV involves the use of a vibrating platform or device that transmits vibrations to the whole body (Hegazy et al., 2021). The parameters used frequently in physical therapy are 0.1-10 mm amplitude and a frequency of 10-120 Hz with session duration ranging between 5 s to 60 min (Saquetto et al., 2015). WBV has been shown to have no effect on stimulating the stretch reflex that makes it a safe and appropriate modality for patients with muscular spasticity (Hopkins et al., 2009).
They are believed to have beneficial effects on muscle function and spasticity. The vibrations stimulate the muscles and joints, promoting muscle function and reducing spasticity (Peungsuwan et al., 2023).
Empirical investigations have yielded promising outcomes concerning the utilization of WBV as a therapeutic modality across various medical conditions. Noteworthy studies have been conducted in diverse clinical contexts, including cerebrovascular accidents (Park et al., 2018), Parkinsonism (Arenales Arauz et al., 2022), Down syndrome (Torres-Nunes et al., 2023), and CP (Hegazy et al., 2021; Peungsuwan et al., 2023), with a particular focus on its efficacy in mitigating spasticity among pediatric patients diagnosed with CP.
For example, Ruck et al. reported a significant increase in the average walking speed measured using a 10-m walking test in addition to improvement in bone mineral density, muscle strength, and function in children with bilateral spastic CP after receiving WBV treatment (Ruck et al., 2010). In a study conducted by Lee and Chon, multiple gait parameters such as gait speed, stride length, and cycle time in addition to ankle range of motion (ROM) demonstrated statistical significant improvement after WBV treatment (Lee and Chon, 2013). A recent study applied WBV on a group of children with spastic CP and reported significant improvements in gross motor functions, gait parameters, and balance in addition to obvious reduction in spasticity of both upper and lower limbs. These improvements were persistent for 12 weeks of follow-up (Tekin and Kavlak, 2021). Other researchers applied a program consisting of WBV and stretching exercises and compared its effects against stretching exercises alone on a sample of children aged 4-12 years on ROM. Beneficial results of joint ROM were reported in the group that received WBV (Ahmadizadeh et al., 2019). These findings highlight the potential therapeutic value of WBV and its promising role in ameliorating the physical manifestations of spasticity and other CP-related signs and symptoms.
It is noteworthy that, despite the growing interest on WBV as a therapeutic tool, the body of empirical evidence, particularly within the context of CP, remains somewhat limited. This paucity of comprehensive evidence has been substantiated by recent studies, including the studies by Saquetto et al. (2015) and Peungsuwan et al. who observed the lack of optimal dose of treatment in the previous literature (Peungsuwan et al., 2023). Additionally, other variations were evident in the previous literature regarding the duration of program, outcomes of interest, and the associated standard treatment (Lee and Chon, 2013; El-Shamy et al., 2014; Saquetto et al., 2015; Stark et al., 2016; Ahmadizadeh et al., 2019; Tekin and Kavlak, 2021; Emara et al., 2022).
In light of this, the primary objective of this review is to conduct a comprehensive assessment of the therapeutic efficacy of WBV interventions specifically within the realm of spastic CP among pediatric patients. This evaluation will extend to key domains, including the impact on muscle tone, functional outcomes, and overall quality of life. By systematically analyzing the available evidence, this review aims to provide valuable insights into the utility and potential limitations of WBV therapy in addressing the multifaceted needs of children afflicted with spastic CP.
METHODOLOGY
The protocol for this systematic review and meta-analysis is registered in the PROSPERO registry (CRD42023455721). The study was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Reporting Items for Systematic Reviews and Meta-Analysis guidelines.
Inclusion criteria
The criteria for inclusion were the following: (i) randomized controlled trials (RCTs); (ii) no age restriction; (iii) sample consisting of subjects having any spastic type of CP; (iv) the intervention of interest was WBV which could be used as a single treatment compared to none, sham, placebo, or other therapeutic interventions; (v) outcomes of interest were muscle tone (spasticity), fine or gross motor function, and quality of life; and (vi) articles published in English.
Information sources
A comprehensive literature search was performed across Scopus (via Science Direct), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO), PubMed, and PEDro, and articles from the year of their inception up to September 2023 were included. Searches were supplemented by manual searching and retrieval of any additional articles meeting eligibility criteria that were cited in reference lists.
Search strategy
Two authors searched the selected databases for the RCTs that met the inclusion criteria. The search keywords were whole-body vibration, WBV, vibration, total body vibration (TBV), spasticity, spastic cerebral palsy, CP, muscle tone, function, quality of life, and randomized controlled trials. Keywords were entered according to the guidelines of each search engine.
Study records
Data management
The records were uploaded to Rayyan QCRI.org (Ouzzani et al., 2016), an Internet-based software that aims to facilitate collaboration among reviewers during the process of eligibility assessment of studies according to the inclusion and exclusion criteria. Before the formal screening process, a calibration exercise was undertaken to pilot and refine the screening procedures and to familiarize the screening team with the Rayyan software.
The team developed a table using Microsoft Excel 2016 to gather the characteristics of eligible studies. Two reviewers were responsible for extracting data reflecting the unique characteristics of each trial. These characteristics included the author’s name, year of publication, the setting, country of study, outcome measures, interventions, sample size, and WBV technique. RevMan software 5.4 was used to manage the data that could be used to conduct the meta-analysis.
Selection process
The Rayyan software was used to assess the studies against the inclusion criteria and refine to remove duplicates. Two authors independently conducted this procedure. In case of uncertainty, the full article was downloaded and reviewed. An e-mail was sent to the corresponding author to obtain the missing or incomplete data. Any disagreement between the reviewers was resolved by a third reviewer. The reasons for exclusion were recorded. The reviewers were blinded to the journal titles, authors of the study, or institutions.
Data collection process
The characteristics of each study are listed using a previously prepared Excel table. The responsible authors were aware of the critical appraisal of clinical trials.
Methodological quality assessment
The PEDro scale for assessment of the quality of the RCTs was used to determine the quality of the included trials. Pedro scale is a valid tool that has been developed to assess the quality of RCTs and is widely used in previous systematic reviews (de Morton, 2009). The score of the quality was extracted directly from the PEDrpo website. For studies not found in the PEDro search engine, the quality was calculated manually using the PEDro quality scale guidelines.
Data synthesis and analysis
Studies investigating similar outcomes and addressing similar interventions in addition to those providing clear quantitative data were grouped and evaluated for heterogeneity. Data were assessed for statistical heterogeneity, which was considered likely if P-values were below 25% obtained on the I 2 statistics (Schiftan et al., 2015). Statistically homogenous trials were subjected to meta-analysis. Meta-analyses were undertaken with RevMan 5.4 using a random-effects model. Sub analyses were conducted to assess the effect of WBV on GMFM-88 D and E categories.
RESULTS
A total of 126 articles were identified from the databases (Table 1). Of these, 18 were removed as duplicates. In total, 108 studies were initially screened for eligibility by reviewing their titles and abstracts. Of these, 96 were excluded and 12 were fully analyzed using the full version. Four studies were excluded due to the use of different study designs (Martakis et al., 2021) and lack of the required outcome measures (Lee and Chon, 2013; Unger et al., 2013; Ali et al., 2019). Two trials were added after searching the reference list of the related studies (Dudoniene et al., 2017; Lee et al., 2019b). The final results included 10 trials (Ahlborg et al., 2006; Ruck et al., 2010; Ibrahim et al., 2014; Stark et al., 2016; Tupimai et al., 2016; Dudoniene et al., 2017; Ahmadizadeh et al., 2019; Lee et al., 2019b; Tekin and Kavlak, 2021; Peungsuwan et al., 2023) as represented in Figure 1. There was good agreement between the reviewers who were responsible for trial inclusion (Kappa = 0.95).
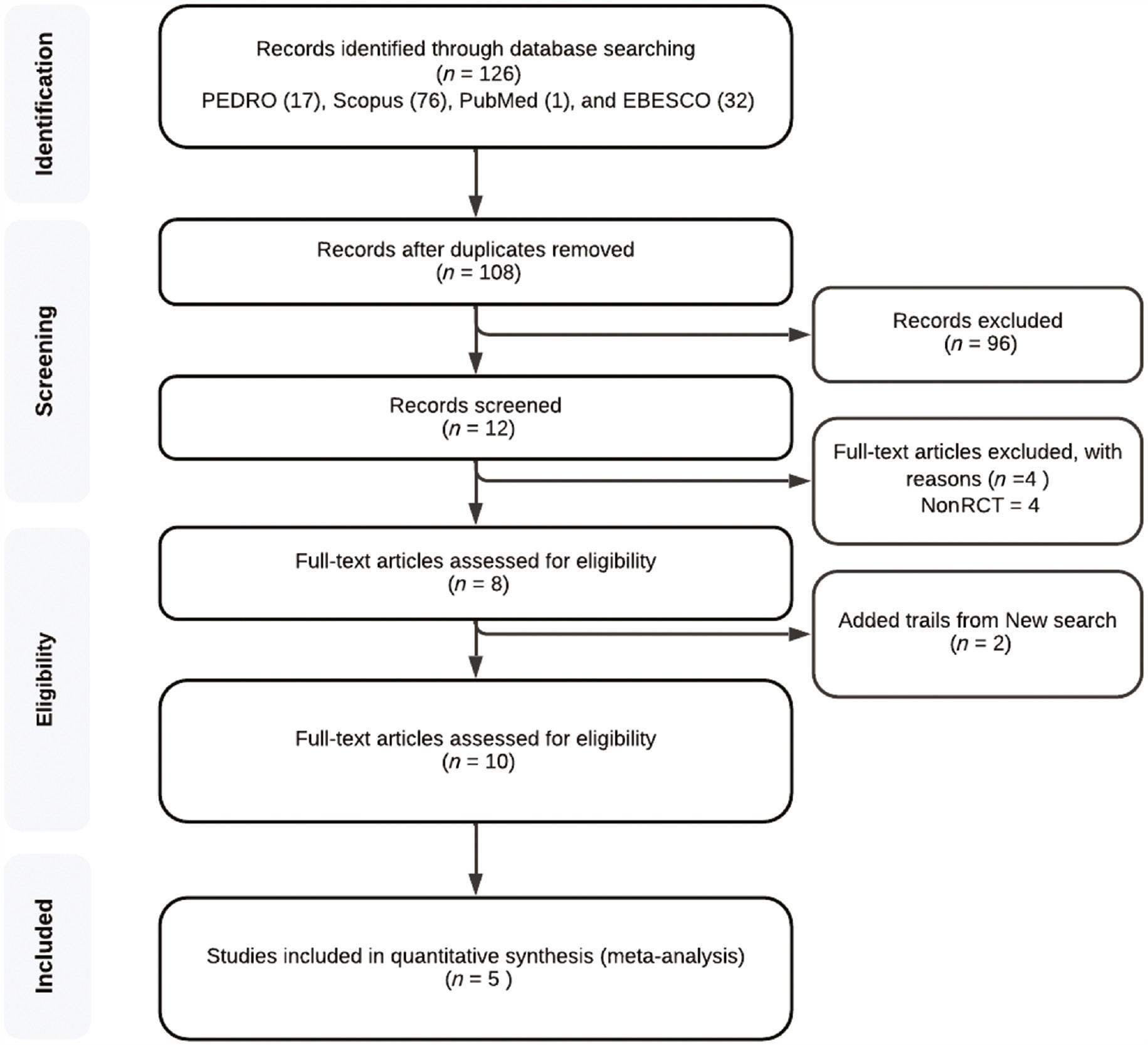
Flow diagram of search strategy, screening, and included studies. Abbreviation: RCT, randomized controlled trial.
Search engines, date of search, and the record for each engine.
| Search database | Date | Number of findings |
|---|---|---|
| PEDro | 22/8/2023 | 17 |
| Scopus | 22/8/2023 | 76 |
| PubMed | 22/8/2023 | 1 |
| EBSCO | 22/8/2023 | 32 |
| Total | 126 |
Characteristics of the included studies
Ten RCTs were included in the current review. These trials investigated the effect of WBV on different outcomes such as function and muscle tone (spasticity). Additionally, other outcomes including gait parameters, muscle mass measured by ultrasonography, joint ROM, clinical tests, and balance were also considered. Meanwhile, none of the included trials assessed the quality of life.
The included trials consisted of 206 participants having spastic CP. Participants’ age ranged between 18 months and 41 years of age. The duration of the intervention varied; the least duration was 3 weeks (Dudoniene et al., 2017) while the longest was 24 weeks (Ruck et al., 2010).
The majority (n = 8) of the trials (Ahlborg et al., 2006; Ruck et al., 2010; Ibrahim et al., 2014; Tupimai et al., 2016; Dudoniene et al., 2017; Ahmadizadeh et al., 2019; Lee et al., 2019a; Tekin and Kavlak, 2021) studied the effects of adding WBV to standard physical therapy. Two trials (Stark et al., 2016; Peungsuwan et al., 2023) compared different protocols of WBV administered to all participating groups. The parameters of WBV varied widely among the trials. For example, Peungsuan et al. (2023) used two different WBV techniques where the first one was static (fixed vibration frequency of 11 Hz) and the second one was characterized by changing vibration frequency (between 7 and 18 Hz). Similarly, Stark et al. used variable vibration frequencies ranging between 12 and 22 Hz (Stark et al., 2016); on the other hand, a fixed frequency (15 Hz) was used by Dudoniene et al. (2017). Regarding the amplitude, some researchers used single amplitude (Stark et al., 2016; Ahmadizadeh et al., 2019; Tekin and Kavlak, 2021) while others used different amplitudes (Ruck et al., 2010; Ibrahim et al., 2014).
Methodological quality and risk of bias assessment
The PEDro scale was used to determine the methodological quality of the included trials as well as the risk of bias. A score of five was used as the cutoff point where any lower score represented a high risk of bias and five or more represented a low risk of bias. Pedroscale has been recommended as a method for assessing risk of bias and demonstrated moderate agreement with the cochrane collaboratibe tool (Moseley et al., 2019). This scale is widely used in systematic reviews. It consists of 11 items, 10 of which were calculated to obtain the final score out of 10. A score below 4 was considered weak, 5-6 was considered fair, 7-8 was considered good, and 9-10 was considered excellent (Table 2).
Methodological quality of the included trials according to the PEDro scale.
| Pedro items | Tekin and Kavlak, 2021 | Stark et al., 2016 | Dudoniene et al., 2017 | Lee et al., 2019 | Ruck et al., 2010 | Ahmedzadah et al., 2019 | Tupimai et al., 2016 | Ibrahim et al., 2014 | Ahlborg et al., 2006 | Peungsuwan et al., 2023 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Eligibility criteria were specified | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2. | Subjects were randomly allocated to groups | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3. | Allocation was concealed | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 4. | The groups were similar at baseline regarding the most important prognostic indicators | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 5. | There was blinding of all subjects | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 6. | There was blinding of all therapists who administered the therapy | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 7. | There was blinding of all assessors who measured at least one key outcome | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| 8. | Measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 |
| 9. | All subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analyzed by “intention to treat” | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10. | The results of between-group statistical comparisons are reported for at least one key outcome | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| 11. | The study provides both point measures and measures of variability for at least one key outcome | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Total score | 4 | 8 | 5 | 6 | 5 | 6 | 4 | 4 | 4 | 6 | |
| Quality | F | G | F | G | F | G | F | F | F | G | |
Abbreviations: G, good; F, fair.
The results of the critical appraisal of the selected studies are presented as a flowchart in Figure 1. Four trials had good methodological quality (Stark et al., 2016; Ahmadizadeh et al., 2019; Lee et al., 2019b; Peungsuwan et al., 2023) and six trials were of fair quality (Ahlborg et al., 2006; Ruck et al., 2010; Ibrahim et al., 2014; Tupimai et al., 2016; Dudoniene et al., 2017; Tekin and Kavlak, 2021). Regarding the risk of bias, four tials showed a high risk of bias (Ahlborg et al., 2006; Ibrahim et al., 2014; Tupimai et al., 2016; Tekin and Kavlak, 2021), while the rest of trials (n = 6) demonstrated a low risk of bias (Ruck et al., 2010; Stark et al., 2016; Dudoniene et al., 2017; Ahmadizadeh et al., 2019; Lee et al., 2019a; Peungsuwan et al., 2023).
It was observed that the included trials have common weak points; the limited number of trials adopted blind design either for the assessor and/or patients, and the concealment of the allocation was conducted in two trials only (Ruck et al., 2010; Stark et al., 2016); no trials except one (Stark et al., 2016) incorporated intention-to-treat strategy in their design. The sample size calculation was conducted in three trials only (Tupimai et al., 2016; Tekin and Kavlak, 2021; Peungsuwan et al., 2023). Two studies conducted follow-up assessments at various points in time (Stark et al., 2016; Ahmadizadeh et al., 2019); finally, the influence of upper limb function and fine motor skills were not studied in the included trials. On the other hand, the majority of the trials (n = 5) reported the intervention-related adverse effect in their findings the adverse effects of the interventions (Ahlborg et al., 2006; Ruck et al., 2010; Ibrahim et al., 2014; Stark et al., 2016; Ahmadizadeh et al., 2019; Peungsuwan et al., 2023).
Meta-analysis
Due to multiple reasons, conducting objective analysis between the included trials was limited. The reasons can be summarized as follows: first, some research introduced the WBV to both the study and control groups (Stark et al., 2016; Peungsuwan et al., 2023); therefore, they cannot be included in the analysis. Second, a single trial did not report any data regarding the desired outcome (spasticity) and they only mentioned the final statistical result (Ahmadizadeh et al., 2019). Lastly, other trials reported the data differently as they mentioned the median, minimum, and maximum values only (Ahlborg et al., 2006) or in the form of median and quartiles (Tupimai et al., 2016).
Only one comparison was conducted, of which five trials (Ruck et al., 2010; Ibrahim et al., 2014; Dudoniene et al., 2017; Lee et al., 2019b; Tekin and Kavlak, 2021) reported consistent data regarding the effect of adding WBV to standard treatment versus standard treatment on gross motor function scales measured by Gross Motor Function Measure (GMFM-88) with its two domains (D and E). The validity and reliability of the GMFM-88 scale were studied and proved in previous work (Josenby et al., 2009; Salavati et al., 2015).
Comparison 1: effect of adding WVB to standard on D values of GMFM-88
As reported in Figure 2, the analysis of the data extracted from the included trials revealed that standard treatment alone was significantly better (P = 0.02) than standard treatment plus WBV on the gross motor D values. However, this finding may be affected by the level of heterogeneity of the included trials (I 2 = 49%). Additionally, four of the five trials (80%) were of fair quality (Table 2), and only one trial (Tekin and Kavlak, 2021) conducted a power test. On the other hand, the basis on which the sample number was selected was not clear in 80% of the trials.
Comparison 2: effect of adding WVB to standard on D values of GMFM-88
As reported in Figure 3, the analysis of the data extracted from the included trials revealed that standard treatment alone was significantly better (P = 0.002) than standard treatment plus WBV on the gross motor E values. The level of heterogeneity of the included trial was acceptable (I 2 = 33%). Additionally, four of the five trials (80%) were of fair quality (Table 1), and only one trial (Tekin and Kavlak, 2021) conducted a power test. On the other hand, the basis on which the sample number was selected was not clear in 80% of the trials.
DISCUSSION
This meta-analysis was conducted to investigate the effects of WBV on muscle tone, function, and quality of life in patients with CP. The primary finding was derived from a single comparison consisting of two trials that assessed gross motor function outcomes in patients receiving standard physical therapy treatment versus those who received the same standard treatment plus WBV.
Previously, two meta-analyses and one systematic review were conducted to study the effectiveness of WBV. While outcomes such as gross motor function were common in all these reviews (Duquette et al., 2015; Saquetto et al., 2015; Cai et al., 2023), spasticity and quality of life were not among the outcomes of interest in these reviews.
Recently, Cai et al. conducted a systematic review and meta-analysis of six studies of different languages and designs (Cai et al., 2023). The outcome of interest included gross motor function, clinical tests such as timed up and go test, six minutes’ walk test, balance, and ROM. According to Cai et al., WBV was better compared to conventional physical therapy in improving the lower-limb motor function which was not supported by the current review. This controversy might be attributed to the fact that the current review included only RCTs, whereas the review by Cai et al. included other types of study designs (Jung et al., 2020). Additionally, two studies published in Chinese language were included in the review by Cai et al., while they were not considered in the current review.
Another meta-analysis was conducted in 2015 where six RCTs were included and two of them were used for quantitative analysis. The outcome of interest in this meta-analysis was the functional level, muscle strength, and lumbar spine bone density (Saquetto et al., 2015). Two comparisons—each of which consisted of two trials—revealed that WBV was more effective than standard treatment on gross motor function in patients with CP. However, the small number of analyzed studies could affect the accuracy of the results.
Duquette et al. (2015) conducted a systematic review to assess the effect of using WBV on different outcomes in patients with CP. Only five studies were subjectively analyzed, where the Scottish intercollegiate guidelines network rating system was used to assess the quality of the studies as well as the risk of bias. In this review, four studies were concerned with children with CP while one study focused on adults. There were one low, four acceptable, and one high-quality studies. According to Duquette et al. lower spasticity levels could be achieved by using WBV.
The findings of the current meta-analysis could be attributed to the heterogeneity of the WBV parameters used in different studies, especially the treatment duration which varied greatly from 3 to 28 weeks. The vibration frequency could inversely affect muscle activity which in turn might decrease the functional ability of the children. The spontaneous recovery and potential to develop may play a role in the difference between the experimental and control interventions. as reported in a previous study (Stark et al., 2016) where the authors found that adding WBV to standard treatment did not have any beneficial effect on the function in patients with CP.
Implication for future research
Future trials should implement high-quality methodological procedures such as blinding, concealment, and sample size calculation. Follow-up protocols should be implemented to evaluate the effects of WBV over time. Studying the effects of WBV on the upper extremity function, ROM, and tone should be addressed in future research.
Future meta-analyses should include a wider range of outcomes including quality of life. Additionally, including studies published in any language might be beneficial in providing more accurate results about the effect of WBV.
Implication for clinical practice
Therapists in clinical practice might find that WBV is beneficial when added to standard treatment as reported in individual studies. However, the current meta-analysis did not suggest that conclusion. Further research of high quality is needed to reach an objective conclusion.
In summary, WBV could be an effective modality in improving variable outcome measures in children with CP. Yet, the limited number of homogenous studies limits the formulation of objective conclusion. The results of the current meta-analysis could add to the bulk of the existing knowledge regarding the efficacy of WBV. It gives the healthcare practitioners as well as the patient and their parents an UpToDate evidence of the use of WBV in treating spasticity associated with CP. This evidence might be useful in improving the quality of intervention through choosing the most effective modalities and enhancing success of therapeutic programs and functional gains for patients. Moreover, the current meta-analysis highlights the strengths and weaknesses of existing studies in addition to the areas that might need further research.
LIMITATION
The current meta-analysis has the following limitations: first, the current work included only trials that were published in scientific journals, and other published materials in conferences were not considered which may affect the results. Articles published in languages other than English Language were not included. Moreover, a limited number of the included trials were of high good quality; none were of high quality. None of the investigated trials studied the long-term effects of WBV. However, CP is a long-term pathology that requires a long rehabilitation period. Finally, outcomes such as quality of life were not considered in all studies.
CONCLUSION
Adding WBV to the standard physical therapy was not superior to standard physical therapy alone in favor of gross motor function in patients with CP. High-quality research examining the effectiveness of whole-body vibration on children with spastic CP exhibiting motor dysfunction is needed.


