- Record: found
- Abstract: found
- Article: found
Comparison of mortality rate and septic and aseptic revisions in total hip arthroplasties for osteoarthritis and femoral neck fracture: an analysis of the German Arthroplasty Registry
Read this article at
Abstract
Background
Indications for total hip arthroplasties (THA) differ from primary osteoarthritis (OA), which allows elective surgery through femoral neck fractures (FNF), which require timely surgical care. The aim of this investigation was to compare mortality and revisions in THA for primary OA and FNF.
Methods
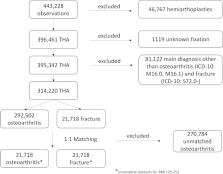
Data collection for this study was performed using the German Arthroplasty Registry (EPRD) with analysis THA for the treatment of FNF and OA. Cases were matched 1:1 according to age, sex, body mass index (BMI), cementation, and the Elixhauser score using Mahalanobis distance matching.
Results
Overall 43,436 cases of THA for the treatment of OA and FNF were analyzed in this study. Mortality was significantly increased in FNF, with 12.6% after 1 year and 36.5% after 5 years compared with 3.0% and 18.7% in OA, respectively ( p < 0.0001). The proportion for septic and aseptic revisions was significantly increased in FNF ( p < 0.0001). Main causes for an aseptic failure were mechanical complications (OA: 1.1%; FNF: 2.4%; p < 0.0001) and periprosthetic fractures (OA: 0.2%; FNF: 0.4%; p = 0.021). As influencing factors for male patients with septic failure ( p < 0.002), increased BMI and Elixhauser comorbidity score and diagnosis of fracture (all p < 0.0001) were identified. For aseptic revision surgeries, BMI, Elixhauser score, and FNF were influencing factors ( p < 0.0001), while all cemented and hybrid cemented THA were associated with a risk reduction for aseptic failure within 90 days after surgery ( p < 0.0001).
Conclusion
In femoral neck fractures treated with THA, a significant higher mortality, as well as septic and aseptic failure rate, was demonstrated compared with prosthesis for the therapy of osteoarthritis. Increased Elixhauser comorbidity score and BMI are the main influencing factors for development of septic or aseptic failure and can represent a potential approach for prevention measures.
Level of evidence: Level III, Prognostic.
Related collections
Most cited references38
- Record: found
- Abstract: not found
- Article: not found
Nonparametric Estimation from Incomplete Observations
- Record: found
- Abstract: found
- Article: not found
A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data.
