- Record: found
- Abstract: found
- Article: found
Incidence of rhabdomyolysis occurrence in psychoactive substances intoxication: a systematic review and meta-analysis
Read this article at
Abstract
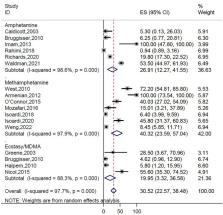
Rhabdomyolysis is a potentially life-threatening condition induced by diverse mechanisms including drugs and toxins. We aimed to investigate the incidence of rhabdomyolysis occurrence in intoxicated patients with psychoactive substances. In this review, three databases (PubMed, Scopus, Web of Science) and search engine (Google Scholar) were searched by various keywords. After the screening of retrieved documents, related data of included studies were extracted and analyzed with weighted mean difference (WMD) in random effect model. The highest incidence of rhabdomyolysis was observed in intoxication with heroin (57.2 [95% CI 22.6–91.8]), amphetamines (30.5 [95% CI 22.6–38.5]), and cocaine (26.6 [95% CI 11.1–42.1]). The pooled effect size for blood urea nitrogen (WMD = 8.78, p = 0.002), creatinine (WMD = 0.44, p < 0.001), and creatinine phosphokinase (WMD = 2590.9, p < 0.001) was high in patients with rhabdomyolysis compared to patients without rhabdomyolysis. Our results showed a high incidence of rhabdomyolysis induced by psychoactive substance intoxication in ICU patients when compared to total wards. Also, the incidence of rhabdomyolysis occurrence was high in ICU patients with heroin and amphetamine intoxication. Therefore, clinicians should anticipate this complication, monitor for rhabdomyolysis, and institute appropriate treatment protocols early in the patient’s clinical course.
Related collections
Most cited references70
- Record: found
- Abstract: found
- Article: not found
Rhabdomyolysis: an evaluation of 475 hospitalized patients.
- Record: found
- Abstract: found
- Article: not found
Rhabdomyolysis: pathogenesis, diagnosis, and treatment.
- Record: found
- Abstract: found
- Article: not found