- Record: found
- Abstract: found
- Article: found
Metabolic Syndrome and Related Factors in Chinese Children and Adolescents: Analysis from a Chinese National Study
Read this article at
Abstract
Aims: Metabolic syndrome (MetS) has become a worldwide epidemic; however, few studies have described its status in Chinese children. This study aimed to estimate MetS status and its associations with geography, economic development, birth weight, and parental education of Chinese children and adolescents.
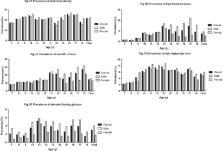
Methods: Data were derived from 15,045 participants aged 7–18 years across seven Chinese provinces. Physical measurement and blood tests were conducted to assess the five classical MetS components described by the International Diabetes Federation, including abdominal obesity (the essential component), high blood pressure, low high-density cholesterol (HDL-C), high triglyceride, and elevated fasting glucose (FG). Logistic regression was adopted to explore possible associations between MetS and other factors.
Results: Overall, MetS prevalence was 2.3%, higher in males (2.8% vs. 1.7% in females), northern regions (3.1%), more developed regions (2.9%), and older participants (aged 16–18 years) ( P < 0.05 for all). Among the five MetS components, abdominal obesity and low HDL-C level were most prevalent (21.8% and 14.4%), and 35.9% of the participants had at least one component. In logistic regression, MetS itself did not correlate with birth weight or parental education. High birth weight was positively correlated with abdominal obesity (odds ratio, 1.48) butnegatively associated with elevated FG (odds ratio, 0.49).
Concusions: MetS itself was not common in Chinese children and adolescents, whereas its certain components were far more prevalent. Children from North China, more-developed areas, and at an older age were more likely to develop MetS. Strategies designed to prevent pediatric MetS in China should focus on prevalent components as well as its geographic and economic development predilections.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship.
- Record: found
- Abstract: found
- Article: not found
Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey.
- Record: found
- Abstract: found
- Article: not found