- Record: found
- Abstract: found
- Article: not found
Underuse of oral anticoagulants in patients with nonvalvular atrial fibrillation in Italy
Read this article at
Abstract
Introduction:
Oral anticoagulants (OAs) are significantly more effective than Aspirin in the prevention of cerebrovascular accidents among patients with atrial fibrillation (AF). Several studies, however, showed OAs to be widely underused in these patients.
Objective:
To assess the appropriateness of antithrombotic therapy in an Italian population of AF patients.
Methods:
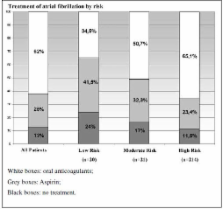
Two hundred and fifty-five consecutive patients affected by nonvalvular AF participated in the study. Data were collected on demographic characteristics, risk factors for stroke, current prophylactic therapy, and perceived or actual risk factors for bleeding. INR levels were measured. Patients were stratified by their risk for stroke (214 at high risk, 21 moderate, 20 low), and their prophylactic therapy was analysed in light of international antithrombotic therapy recommendations. After therapy adjustment, 203 of our patients were followed-up for the occurrence of cerebrovascular events for an average of 27 months.
Results:
Upon admission, 35% ( n=75) of patients in the high-risk category were either taking no antithrombotic prophylaxis or were being treated with Aspirin. In addition, 38 of 139 patients receiving OAs had an INR<2. Thus, a total of 113 (52.8%) high-risk subjects were not receiving adequate antithrombotic therapy. Of high-risk patients not treated with OAs, 46.7% reported no perceived or actual risk factors for bleeding. The annual incidence of cerebrovascular accidents was 3.8% among 163 high-risk patients assigned to OA treatment, and 4.5% among 39 patients given Aspirin treatment. Relative to expected annual incidence rates, cerebrovascular risk in anticoagulated patients was reduced by about 70%.
Related collections
Most cited references40
- Record: found
- Abstract: found
- Article: not found
Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis.
- Record: found
- Abstract: found
- Article: not found
Warfarin in the prevention of stroke associated with nonrheumatic atrial fibrillation. Veterans Affairs Stroke Prevention in Nonrheumatic Atrial Fibrillation Investigators.
- Record: found
- Abstract: found
- Article: not found
