- Record: found
- Abstract: found
- Article: found
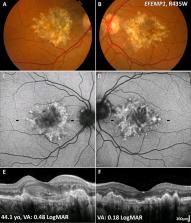
Macular dystrophies: clinical and imaging features, molecular genetics and therapeutic options
Abstract
Macular dystrophies (MDs) consist of a heterogeneous group of disorders that are characterised by bilateral symmetrical central visual loss. Advances in genetic testing over the last decade have led to improved knowledge of the underlying molecular basis. The developments in high-resolution multimodal retinal imaging have also transformed our ability to make accurate and more timely diagnoses and more sensitive quantitative assessment of disease progression, and allowed the design of optimised clinical trial endpoints for novel therapeutic interventions. The aim of this review was to provide an update on MDs, including Stargardt disease, Best disease, X-linked r etinoschisis, pattern dystrophy, Sorsby fundus dystrophy and autosomal dominant drusen. It highlights the range of innovations in retinal imaging, genotype–phenotype and structure–function associations, animal models of disease and the multiple treatment strategies that are currently in clinical trial or planned in the near future, which are anticipated to lead to significant changes in the management of patients with MDs.
Related collections
Most cited references98
- Record: found
- Abstract: found
- Article: not found
Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt's macular dystrophy: follow-up of two open-label phase 1/2 studies

- Record: found
- Abstract: found
- Article: found
Transplantation of Human Embryonic Stem Cell-Derived Retinal Pigment Epithelial Cells in Macular Degeneration
- Record: found
- Abstract: found
- Article: found