- Record: found
- Abstract: found
- Article: found
Culture and PCR based detection of bacteria causing urinary tract infection in urine specimen
Read this article at
Abstract
Objectives:
Urinary tract infections are the second most common bacterial infections occurring at all ages and both sexes. The increasing rate of antibiotic resistance is a global concern. The use of routinely used antibiotics is resulting in treatment failure. The objective of this study was to diagnose the urinary tract infections by routine culture sensitivity test and by molecular methods.
Methods:
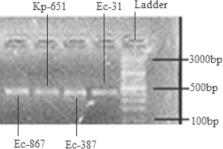
This study was conducted in Microbiology laboratory, Bolan Medical Complex Hospital, Quetta, from July 1 st to 31 st March 2019. Isolates were identified biochemically by API20E & API20NE. Antibiogram was performed using disc diffusion Kirby Bauer technique. The 16S rDNA gene approach was used for molecular identification of bacterial isolates. The presence of the bla NDM-1 gene was identified by polymerase chain reaction (PCR).
Results:
We isolated 146 bacterial isolates namely Escherichia coli (n=99) 67.80%, Klebsiella pneumoniae (n=33) 22.60%, Pseudomonas aeruginosa (n=11) 7.53% and Proteus mirabilis (n=3) 2.05% from 2032 urine samples. The resistance pattern was dominated by Multi Drug Resistance (MDR). Remarkably, four isolates of Escherichia coli (n=3) and Klebsiella pneumoniae (n=1) were displaying resistance against a range of antibiotics used in the study, including carbapenems but sensitive to tigecycline and polymyxins only, suggesting extensive drug resistance having bla NDM-1 gene.
Conclusion:
This is the first report on direct molecular detection of bacterial pathogens from urinary tract infected patients in Balochistan. The presence of bla NDM-1 in different bacterial species and their extensive drug resistance pattern poses a significant clinical threat. Molecular detection of bacteria and resistant gene may reduce the diagnostic time of patients.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
16S ribosomal DNA amplification for phylogenetic study.
- Record: found
- Abstract: found
- Article: not found
Laboratory diagnosis of urinary tract infections in adult patients.
- Record: found
- Abstract: found
- Article: not found