- Record: found
- Abstract: found
- Article: found
Effectiveness and safety of thymectomy plus prednisone compares with prednisone monotherapy for the treatment of non-thymomatous Myasthenia Gravis : Protocol for a systematic review
Read this article at
Abstract
Background:
The pathogenesis of myasthenia gravis (MG) has strong connection with thymic abnormalities. Thymic hyperplasia or thymoma can be found with most patients. Thymectomy is currently one of the regular treatment in clinic, which is, however, still controversial for non-thymomatous MG. This research will assess the effectiveness and safety of thymectomy plus prednisone compared to prednisone monotherapy for the treatment of non-thymomatous MG systematically.
Methods:
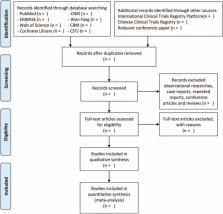
According to eligibility and ineligibility criteria, 8 databases, including PubMed, EMBASE, the Web of Science, the Cochrane Library, China National Knowledge Infrastructure (CNKI), Wan-fang Database, Chinese Biomedical Literature Database (CBM), China Science and Technology Journal Database (CSTJ), will be searched to gather the up-to-standard articles from September 2000 to September 2025. Inclusion criteria are as follows: randomized controlled trials of thymectomy plus prednisone for the treatment of non-thymomatous MG. The quantitative myasthenia gravis score (QMG) and the dose of prednisone required will be accepted as the main outcomes. Data synthesis, subgroup analysis, sensitivity analysis, and meta-regression analysis will be conducted using RevMan 5.3 software. We will use Egger or Begg test to evaluate symmetry on a funnel plot which is made to assess reporting bias, and use trial sequential analysis (TSA) to exclude the probability of false positives.
Results:
This systematic review will measure the QMG and the dose of prednisone required, the myasthenia gravis activities of daily living scale scores (MG-ADL), treatment-associated complications, incidence of myasthenic crisis and other aspects to comprehensively assess the clinical benefits of thymectomy plus prednisone for MG patients without thymoma.
Related collections
Most cited references18

- Record: found
- Abstract: found
- Article: found
A systematic review of population based epidemiological studies in Myasthenia Gravis
- Record: found
- Abstract: not found
- Article: not found
Myasthenia gravis: Recommendations for clinical research standards

- Record: found
- Abstract: found
- Article: found