- Record: found
- Abstract: found
- Article: found
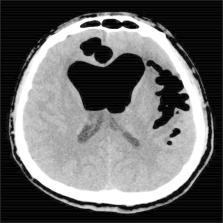
Tension Pneumocephalus from Endoscopic Endonasal Surgery: A Case Series and Literature Review
Abstract
Purpose
Tension pneumocephalus (TP) caused by endoscopic endonasal surgery is a serious complication. We report four cases of TP caused by endoscopic surgery and review other cases in the literature, with special attention devoted to symptoms, imaging features, and therapeutic approaches.
Methods
A retrospective chart review of patients who experienced TP caused by endoscopic surgery in our institution between 2015 and 2018 was performed. Additionally, the MEDLINE database was searched for all case series or reports of TP caused by endoscopic surgery.
Results
Eighteen articles were identified for review, including four cases from the authors’ institution; ultimately, 26 cases were included in the present study. The main symptoms of TP were headache and a change in mental status. Cerebrospinal fluid (CSF) leakage was reported in 21 of the 26 patients (80.8%). Eight of the 26 patients (30.8%) presented with the “Mount Fuji sign” imaging feature. Twenty-four patients were treated with surgical intervention for TP (endoscopic multilayer closure of skull base defect, cranial burr hole, or bifrontal craniotomy). In addition, the present study is the first to report two patients with TP who were successfully treated conservatively.
Conclusion
The therapeutic method for treating TP should depend on the degree of the mass effect and clinical symptoms. When patients with TP present with obvious symptoms of CSF leakage and intracranial hypertension, urgent surgical multilayer repair of the skull base defects and/or release of the intracranial pressure are keys to treating these patients. However, conservative treatment under close observation is also feasible when the related symptoms are not overtly obvious.
Most cited references25

- Record: found
- Abstract: found
- Article: found
Traumatic tension pneumocephalus – Two cases and comprehensive review of literature
- Record: found
- Abstract: found
- Article: not found
Treatment of pneumocephalus after endoscopic sinus and microscopic skull base surgery.
