- Record: found
- Abstract: found
- Article: found
Prevalence of Malaria Infection and Risk Factors Associated with Anaemia among Pregnant Women in Semiurban Community of Hazaribag, Jharkhand, India
Read this article at
Abstract
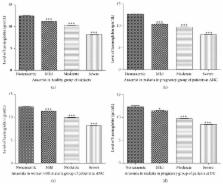
The escalating burden, pathogenesis, and clinical sequel of malaria during pregnancy have combinatorial adverse impact on both mother and foetus that further perplexed the situation of diagnosis, treatment, and prevention. This prompted us to evaluate the status of population at risk of MIP in Hazaribag, Jharkhand, India. Cross-sectional study was conducted over a year at Sadar Hospital, Hazaribag. Malaria was screened using blood smear and/or RDT. Anaemia was defined as haemoglobin concentration. Pretested questionnaires were used to gather sociodemographic, clinical, and obstetrical data. The prevalence of MIP was 5.4% and 4.3% at ANC and DU, and 13.2% malaria was in women without pregnancy. Interestingly, majority were asymptomatically infected with P. vivax (over 85%) at ANC and DU. Peripheral parasitemia was significantly associated with fever within past week, rural origin of subjects, and first/second pregnancies in multivariate analysis, with the highest risk factor associated with fever followed by rural residence. Strikingly in cohort, anaemia was prevalent in 86% at ANC as compared to 72% at DU, whereas severe anaemia was 13.6% and 7.8% at ANC and DU. Even more anaemia prevalence was observed in MIP group (88% and 89% at ANC and DU), whereas severe anaemia was 23% and 21%, respectively. In view of observed impact of anaemia, parasitemia and asymptomatic infection of P. vivax during pregnancy and delivery suggest prompt diagnosis regardless of symptoms and comprehensive drug regime should be offered to pregnant women in association with existing measures in clinical spectrum of MIP, delivery, and its outcome.
Related collections
Most cited references62
- Record: found
- Abstract: found
- Article: not found
The global distribution of clinical episodes of Plasmodium falciparum malaria.
- Record: found
- Abstract: found
- Article: not found