- Record: found
- Abstract: found
- Article: found
Basal Cell Carcinoma Presenting as a Perianal Ulcer and Treated with Radiotherapy
letter
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Dear Editor:
Basal cell carcinoma (BCC) in the perianal and genital areas accounts for <1% of all
BCCs1. If the patient is unsuitable or unwilling to receive surgical treatment, topical
photodynamic therapy and radiotherapy can be considered alternative treatment options2.
In this report, we describe a case of BCC that presented as a perianal ulcer and showed
a good response to radiotherapy.
An 83-year-old man presented with an erythematous ulcer on his perianal area for 3~4
years. The skin lesion was slowly growing, but did not cause pain or bleeding. He
did not report any gastrointestinal symptoms. He had a medical history of hypertension,
diabetes mellitus, subarachnoid hemorrhage.
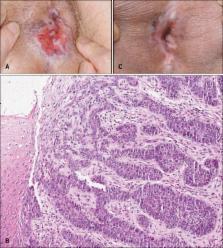
On examination, a single 3.0×3.0 cm-sized, erythematous, asymptomatic ulcer with raised
edges was observed on the perianal area (Fig. 1A). Under the clinical impression of
Paget disease or Crohn disease, punch biopsy was performed. Histopathologically, nodular
masses of basaloid cells extended into the dermis and showed a peripheral palisading
pattern, which were consistent with BCC (Fig. 1B).
He decided to undergo radiotherapy due to the high operative risk associated with
his old age and history of subarachnoid hemorrhage. He received 3 Gy per fraction
for 3 times a week for a total dose of 51 Gy over 17 fractions. At the end of radiotherapy,
no acute radiogenic skin toxicities such as erythema and desquamation were noted.
Two months after radiotherapy, the ulcerative lesion showed considerable clinical
improvement (Fig. 1C) and still showed no aggravation after 5 month follow-up. The
patient refused to undergo an additional skin biopsy; therefore, he scheduled regular
follow-up visits.
BCC of non-sun-exposed areas is extremely rare. Among the anogenital BCC, the pubis
is the most common, followed by the perianal area, the scrotum, and the penis1. Clinical
appearance ranged from erythematous papules to noduloplaques, and ulcers. According
to a previous report that reviewed 51 anogenital BCCs, ulcerated lesions were seen
in 15 cases (29.4%)1.
Perianal ulcerative BCC may initially be misdiagnosed as a benign dermatologic or
gastrointestinal disease. Perianal Paget disease, cutaneous metastasis of gastrointestinal
malignancy and Crohn disease should be excluded3.
Radiotherapy can be a treatment option in elderly patients and those with significant
medical comorbidities4. In the present case, poor medical conditions and the location,
which made it difficult for complete excision, rendered him unsuitable for surgery.
However, patients treated with radiotherapy should be closely followed up because
BCC treated with radiotherapy recurs more often than that treated with Mohs micrographic
surgery; Rowe et al.5 reported that the 5-year recurrence rate of radiotherapy-treated
disease is higher (9.8%) than that of Mohs micrographic surgery (5.6%). Also, the
potential for radiogenic toxicity in the skin should not be ignored, especially when
it might cause severe functional discomfort.
In summary, we describe a rare case of BCC that presented as a perianal ulcer. Dermatologists
should consider BCC in the differential diagnosis of a painless, ulcerated lesion
on the perianal area. We also suggest considering radiotherapy in cases of BCC in
the perianal area when surgical treatment is not possible.
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
Mohs surgery is the treatment of choice for recurrent (previously treated) basal cell carcinoma.
June Carroll, Laurence Rowe, Alexander Day (1989)
- Record: found
- Abstract: found
- Article: not found
Cutaneous manifestations of gastrointestinal disease: part I.
Kejal R Shah, C. Boland, Mahir Patel … (2013)
- Record: found
- Abstract: found
- Article: not found
Perianal and genital basal cell carcinoma: A clinicopathologic review of 51 cases.
Peter G Gibson, Mustafa Ahmed (2001)