- Record: found
- Abstract: found
- Article: found
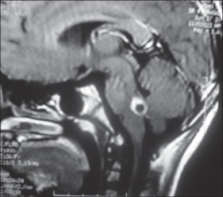
Neurocysticercosis presenting as Millard Gubler syndrome
case-report
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Neurocysticercosis is a common childhood neurological illness in India. A variety of presentations have been reported in the literature, including weber syndrome. Neurocysticercosis, manifesting as Millard Gubler syndrome, have not been reported in literature. Therefore, we report a child presented to us with Millard Gubler syndrome due to pontomedullary neurocysticercosis and was treated successfully.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: not found
Proposed diagnostic criteria for neurocysticercosis.
V Rajshekhar, Stimson P Schantz, O Del Maschio … (2001)
- Record: found
- Abstract: found
- Article: not found
Clinical spectrum of 500 children with neurocysticercosis and response to albendazole therapy.
- Record: found
- Abstract: found
- Article: not found
Neurocysticercosis: a review.
Larry Hawk, Fabian Theis, Kiarash Shahlaie … (2005)