- Record: found
- Abstract: found
- Article: found
Comparison of 4 mg dexamethasone versus 8 mg dexamethasone as an adjuvant to levobupivacaine in fascia iliaca block-a prospective study
Read this article at
Abstract
Background
To compare the effects of adding two different doses of dexamethasone on the duration and quality of the fascia iliaca block in patients undergoing proximal femoral fracture surgery.
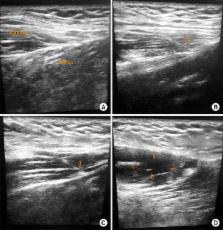
Methods
A total of 60 patients (age 18–70 years) undergoing proximal femoral nailing surgery under spinal anesthesia were given fascia iliaca block after random assignment to one of the two groups: Group H received an injection of levobupivacaine (0.5%) 28 ml with 2 ml (8 mg) dexamethasone, and Group L received an injection of levobupivacaine (0.5%) 28 ml with dexamethasone 1 ml (4 mg) with 1 ml normal saline. Assessment of the duration of analgesia and the total tramadol requirement over 48 hours were noted after a successful block.
Results
The duration of analgesia was found to be significantly longer in Group H (17.02 ± 0.45 h) than in the Group L patients (14.29 ± 0.45 h) with a p-value of 0.000. Postoperative analgesic requirement (amount of tramadol in mg) was significantly higher in Group L (Q2: 200.0; IQR: 100.0, 200.0) as compared to Group H (Q2: 100.0; IQR: 100.0, 200.0) with a p-value of 0.034. No patient showed any sign of neurotoxicity.
Conclusions
Dexamethasone, in a dose of 8 mg, is superior to 4 mg when used as an adjuvant with levobupivacaine in the FIB. Though both prolonged analgesia and were effective in reducing oral/intravenous analgesics, 8 mg dexamethasone can be recommended as a more efficacious adjuvant to local anesthetics in the FIB.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Local corticosteroid application blocks transmission in normal nociceptive C-fibres.
- Record: found
- Abstract: found
- Article: not found
Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials.
- Record: found
- Abstract: found
- Article: not found