- Record: found
- Abstract: found
- Article: found
Risk factors for human papillomavirus infection prevalent among Uyghur women from Xinjiang, China
Read this article at
Abstract
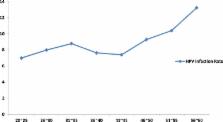
We investigated the incidence of HPV and risk factors for infection among rural Uyghur women in the Xinjiang province of northwestern China, where there is a high incidence of cervical cancer. We used the careHPV kit to test 6000 sexually active Uyghur women aged 21 to 60 years for HPV, and conducted a comprehensive questionnaire survey to identify relevant HPV infection factors. Our data show the HPV infection rate to be 8.42%, which is lower than 11.7% reported worldwide, despite the higher cervical cancer incidence. Multivariate logistic regression revealed that Uyghur women that had (a) poor personal hygiene and care; (b) no previous gynecological examination; (c) a higher education level; (d) unprotected sex and inadequate personal hygiene; (e) used their fingers for vaginal cleaning (f) smoking husbands and (j) used sanitary napkins or toilet paper during menstruation or used clod as the bathroom wipe material were at greater risk for HPV infection. This suggests that proper interventions that improve personal hygiene, including not using ones fingers for vaginal cleaning, use of condoms, regular gynecological exams and a reduction in smoking by spouses could lower the cervical cancer risk by lowering HPV infection rates. In addition, increasing awareness among more educated women regarding HPV and implementation of effective interventions could reduce the risk of HPV infection in Uyghur women.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Worldwide distribution of human papillomavirus types in cytologically normal women in the International Agency for Research on Cancer HPV prevalence surveys: a pooled analysis.
- Record: found
- Abstract: found
- Article: not found
Role of parity and human papillomavirus in cervical cancer: the IARC multicentric case-control study.
- Record: found
- Abstract: found
- Article: not found