- Record: found
- Abstract: found
- Article: found
Transplant-associated Kaposi’s sarcoma in a kidney allograft: a case report
Read this article at
Abstract
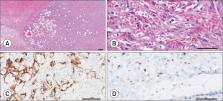
Kaposi’s sarcoma (KS) is a disease that is not widely known among the general public, but has a high prevalence among organ transplant recipients. Here, we present a rare case of intragraft KS after kidney transplantation. A 53-year-old woman who had been on hemodialysis due to diabetic nephropathy underwent deceased-donor kidney transplantation on December 7, 2021. Approximately 10 weeks after kidney transplantation, her creatinine level increased to 2.99 mg/dL. Upon examination, ureter kinking was confirmed between the ureter orifices and the transplanted kidney. As a result, percutaneous nephrostomy was performed, and a ureteral stent was inserted. During the procedure, bleeding occurred due to a renal artery branch injury, and embolization was performed immediately. Subsequently, kidney necrosis and uncontrolled fever developed, leading to graftectomy. Surgical findings revealed that the kidney parenchyma was necrotic as a whole, and lymphoproliferative lesions had formed diffusely around the iliac artery. These lesions were removed during graftectomy, and a histological examination was performed. The kidney graft and lymphoproliferative lesions were diagnosed as KS based on a histological examination. We report a rare case in which a recipient developed KS in the kidney allograft as well as in adjacent lymph nodes.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Kaposi sarcoma
- Record: found
- Abstract: found
- Article: not found
Sirolimus for Kaposi's sarcoma in renal-transplant recipients.
- Record: found
- Abstract: not found
- Article: not found