- Record: found
- Abstract: found
- Article: found
Rapidly Progressing Generalized Morphea with High Lyme Disease Titer
letter
Mi Soo Choi ,
Gi Hyun Seong
1 ,
Myeong Jin Park
1 ,
Minkee Park
1 ,
Seung Phil Hong
1 ,
Byung Cheol Park
1 ,
Myung Hwa Kim
1
Sep-Oct 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Sir,
A 51-year-old male presented with erythematous to brownish ill-defined indurated enlarging
plaques on the right leg, left flank, and left anterior chest over 10 days with hardness.
All of the lesions were exceeding 5 cm in diameter [Figures 1 and 2]. He did not give
tick bite history and never had traveled to the endemic areas of Lyme borreliosis.
Biopsy from the right leg showed lymphoplasmacytic infiltrate and fibrosis in the
dermis and subcutis [Figures 3 and 4]. Complete blood count, chemistry, HIV testing
were normal, and antinuclear antibody, anti-Ro/La, anti-RNP, anti Scl70, anti-centromere
antibody were all negative. Lyme disease immunoglobulin G titer was 1:512 and IgM
titer was <1:16 in immunofluorescence assay (IFA), but negative in Western blot test.
Warthin Starry stain was negative. DNA was not detected in polymerase chain reaction.
Figure 1
Erythematous to brown colored, irregularly circumscribed indurated plaques are found
from upper thigh to calf
Figure 2
Slightly whitish to erythematous irregular shaped indurated patch on chest, around
nipple
Figure 3
Histopathology of specimen from right calf shows perivascular and interstitial infiltrates
of lymphocytes and plasma cells in dermis (H and E, ×40)
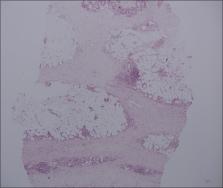
Figure 4
Patchy fibrosis in the subcutaneous layer, and lymphoplasmacytic infiltrates are found.
Trabeculae are thickened in subcutaneous layer (H and E, ×100)
Transthoracic echocardiography, electrocardiography, esophagogastroduodenoscopy, colonofibroscopy,
chest and abdominopelvic computed tomography, and pulmonary function test were done
and all were normal. Oral doxycycline (200 mg/day) for 3 weeks was started due to
the possibility of Lyme borreliosis but without response. After systemic corticosteroid
administration, the progression was slowed. After discontinuing the medication for
3 months, new skin lesions were found on the left buttock and thigh. Corticosteroid
was started again, and the progression was stopped. There was no progression after
cessation of medication until reporting.
Follow-up IFA and western blot determinations were performed 6 months after the onset
of symptom, but the titer did not decrease, and western blot was still negative.
Lyme disease, also known as Lyme borreliosis, is a multi-organ infection caused by
spirochetes of the Borrelia burgdorferi sensu lato group which are transmitted by
ticks of the species Ixodes.[1] Common skin manifestations include erythema migrans,
lymphocytoma, and acrodermatitis chronica atrophicans.[1] Recently, there have been
some reports linking morphea or lichen sclerosus to B. burgdorferi infection.[1]
The presence of antibodies to B. burgdorferi in 50% of patients with morphea was found
with enzyme-linked immunosorbent assay (ELISA),[1] but contradictory data have been
proposed.[2] Most reports of the association between positive antibody test to B.
burgdorferi and morphea come from Europe, and have been rarely found in the USA.[3]
Differences between Borrelia strains and prevalence in the USA and in Europe have
been raised to explain these conflicting results.[3] B. garinii, B. afzelii, and B.
burgdorferi sensu stricto are present in Europe, only B. burgdorferi sensu stricto
is identified in the USA. It has been suggested that only certain types of infection
of B. burgdorferi may lead to morphea. B. burgdorferi sensu stricto, has never been
found in late dermatologic manifestations of Lyme borreliosis, this may explain the
reason of conflicting data from different regions.[3]
The overall false-positive rate of Lyme borreliosis testing is approximately 5%.[4]
When patients have other viral or spirochetal infections or autoimmune diseases, false-positive
findings with ELISA or IFA may occur.[4] There has been only one case of morphea with
false positivity to Lyme titer since 1993.[5] We experienced this interesting case
of rapidly progressing generalized morphea with high antibody titer to B. burgdorferi.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
In the form the patient(s) has/have given his/her/their consent for his/her/their
images and other clinical information to be reported in the journal. The patients
understand that their names and initials will not be published and due efforts will
be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
Cross-reactivity of nonspecific treponemal antibody in serologic tests for Lyme disease.
L A Magnarelli, J N Miller, J Anderson … (1990)
- Record: found
- Abstract: found
- Article: not found
Is morphoea caused by Borrelia burgdorferi? A review.
B Weide, T Walz, James Garbe (2000)
- Record: found
- Abstract: found
- Article: not found
Detection of Borrelia burgdorferi DNA (B garinii or B afzelii) in morphea and lichen sclerosus et atrophicus tissues of German and Japanese but not of US patients.
H Fujiwara, Takahiro Fujiwara, K Hashimoto … (1997)
Author and article information
Comments
Comment on this article
scite_
Similar content321
- Lyme borreliosis.Authors: Gerold Stanek, Franc Strle