- Record: found
- Abstract: found
- Article: found
Mental health and well-being from childhood to adulthood: design, methods and results of the 11-year follow-up of the BELLA study
Read this article at
Abstract
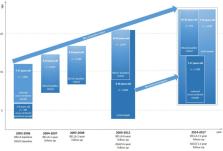
Mental health and well-being are of great interest in health policy and research. Longitudinal surveys are needed to provide solid population-based data. We describe the design and methods of an 11-year follow-up of the German BELLA study in children, adolescents and young adults, and we report on age- and gender-specific courses of general health and well-being, long-term health-related outcomes of mental health problems, and mental health care use. The BELLA study is the module on mental health and well-being within the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Standardised measures were used at each of the five measurement points of the BELLA study. In the 11-year follow-up, young people aged 7–31 years participated ( n = 3492). Individual growth modelling, linear regression and descriptive analyses were conducted. Self-reported general health and well-being were both better in younger (vs. older) and in male (vs. female) participants according to the data from all five measurement points. Mental health problems in childhood and adolescence (measured at baseline) predicted impaired health outcomes at 6-year and 11-year follow-ups. Approximately one out of four children with a diagnosed mental disorder was not undergoing mental health treatment. With its 11-year follow-up, the prospective longitudinal BELLA study provides new and solid data on mental health and well-being from childhood to adulthood in Germany, and these data are important for health promotion and prevention practices. These results are consistent with previous findings. Promising future analyses are planned.
Related collections
Most cited references87
- Record: found
- Abstract: not found
- Article: not found
The CES-D Scale: A Self-Report Depression Scale for Research in the General Population
- Record: found
- Abstract: found
- Article: not found
Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication.
- Record: found
- Abstract: found
- Article: not found