- Record: found
- Abstract: found
- Article: found
Biomechanical effect of intertrochanteric curved varus osteotomy on stress reduction in femoral head osteonecrosis: a finite element analysis
Read this article at
Abstract
Background
Intertrochanteric curved varus osteotomy (CVO) has been widely used to remove the necrotic bone away from the weight-bearing portion in the treatment of osteonecrosis of the femoral head (ONFH). However, whether all types of necrosis will benefit from CVO, in terms of the stress level, the effect of different center-edge (CE) angles of acetabulum on stress distribution of necrosis after CVO, and the relationship between the intact ratio and the stress of necrosis, has never been addressed. The purpose of the study was to evaluate the influence of CVO on the stress reduction in necrotic bone using a finite element analysis (FEA) with different CE angles.
Methods
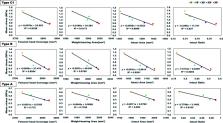
CVO finite element models of the hip joint were simulated with a lesion of 60°. The osteotomy angles were divided into four configurations (15°, 20°, 25°, and 30°), and three types (A, B, and C1) of lesions were established based on the Japanese Investigation Committee (JIC) classification. In addition, two CE angles (18° and 33°) of acetabulum were considered. The maximum and mean von Mises stress were analyzed in terms of the necrotic bone by a physiological loading condition. Moreover, the correlation of the intact ratio measured in 3D and the stress distribution after CVO was analyzed.
Results
Stress reduction was obtained after CVO. For type B, the CVO angle was 20° (0.61 MPa), and for type C1, the CVO angle was 30° (0.77 MPa), if the mean stress level was close to type A (0.61 MPa), as a standard. The maximum and mean von Mises stress were higher in the CE angle of 18°models, respectively. The intact ratio measured in 3D had a good negative correlation with stress after CVO and had more influence on stress distribution in comparison to other geometric parameters.
Conclusions
For making decisions about the biomechanics of CVO, a CVO angle of > 20° was recommended for type B and > 30° was safe for type C1. The risk of progressive collapse was increased in the insufficient situation of the weight-bearing portion after CVO. The intact ratio could provide information about clinical outcomes and stress distribution after CVO.
Related collections
Most cited references49
- Record: found
- Abstract: found
- Article: not found
Is my model good enough? Best practices for verification and validation of musculoskeletal models and simulations of movement.
- Record: found
- Abstract: found
- Article: not found
Trabecular bone modulus-density relationships depend on anatomic site.
- Record: found
- Abstract: found
- Article: not found