- Record: found
- Abstract: found
- Article: found
First-degree relatives of cancer patients: a target group for primary prevention? A cross-sectional study
Read this article at
Abstract
Background
Persons with a first-degree relative (FDR) with cancer are at increased cancer risk. We investigated preventive behaviour, cancer risk perception and readiness to change an unhealthy lifestyle in persons with and without an FDR with cancer.
Methods
Using an online questionnaire, we conducted a cross-sectional study in Germany including persons (≥35 years) with an FDR with colorectal, lung, prostate, breast, stomach or cervical/uterine cancer ( n = 621) and persons without cancer in FDRs ( n = 303). Quota sampling ensured similar age and sex distributions in both groups.
Results
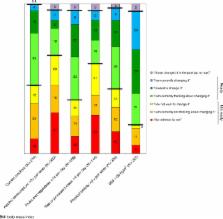
Unfavourable lifestyle factors were equally common in both groups. The proportion perceiving an increased cancer risk significantly differed ( p < 0.0001) with 4% among respondents without cancer in FDRs and 18% (colorectal cancer) to 30% (stomach cancer) among cancer patients’ relatives. The proportion of smokers ready to quit smoking was significantly higher among those perceiving an increased vs. a lower cancer risk (64 vs. 46%, p = 0.04). There was a similar association for readiness to increase physical activity and consumption of fruits/vegetables and to reduce alcohol consumption.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Unrealistic optimism about susceptibility to health problems.
- Record: found
- Abstract: found
- Article: not found
Environmental and heritable causes of cancer among 9.6 million individuals in the Swedish Family-Cancer Database.
- Record: found
- Abstract: found
- Article: not found