- Record: found
- Abstract: found
- Article: found
Mode of Death after Extracorporeal Cardiopulmonary Resuscitation
Read this article at
Abstract
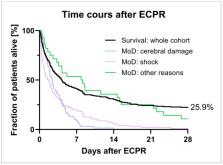
Introduction: Extracorporeal cardiopulmonary resuscitation (ECPR) might be a lifesaving therapy for patients with cardiac arrest and no return of spontaneous circulation during advanced life support. However, even with ECPR, mortality of these severely sick patients is high. Little is known on the exact mode of death in these patients. Methods: Retrospective registry analysis of all consecutive patients undergoing ECPR between May 2011 and May 2020 at a single center. Mode of death was judged by two researchers. Results: A total of 274 ECPR cases were included (age 60.0 years, 47.1% shockable initial rhythm, median time-to-extracorporeal membrane oxygenation (ECMO) 53.8min, hospital survival 25.9%). The 71 survivors had shorter time-to-ECMO durations (46.0 ± 27.9 vs. 56.6 ± 28.8min, p < 0.01), lower initial lactate levels (7.9 ± 4.5 vs. 11.6 ± 8.4 mg/dL, p < 0.01), higher PREDICT-6h (41.7 ± 17.0% vs. 25.3 ± 19.0%, p < 0.01), and SAVE (0.4 ± 4.8 vs. −0.8 ± 4.4, p < 0.01) scores. Most common mode of death in 203 deceased patients was therapy resistant shock in 105/203 (51.7%) and anoxic brain injury in 69/203 (34.0%). Comparing patients deceased with shock to those with cerebral damage, patients with shock were significantly older (63.2 ± 11.5 vs. 54.3 ± 16.5 years, p < 0.01), more frequently resuscitated in-hospital (64.4% vs. 29.9%, p < 0.01) and had shorter time-to-ECMO durations (52.3 ± 26.8 vs. 69.3 ± 29.1min p < 0.01). Conclusions: Most patients after ECPR decease due to refractory shock. Older patients with in-hospital cardiac arrest might be prone to development of refractory shock. Only a minority die from cerebral damage. Research should focus on preventing post-CPR shock and treating the shock in these patients.
Related collections
Most cited references29
- Record: found
- Abstract: not found
- Article: not found
2018 ESC/EACTS Guidelines on myocardial revascularization
- Record: found
- Abstract: found
- Article: not found
Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care.

- Record: found
- Abstract: found
- Article: found