- Record: found
- Abstract: found
- Article: found
Migraine, vascular risk, and cardiovascular events in women: prospective cohort study
Read this article at
Abstract
Objectives To evaluate whether the association between migraine with aura and increased risk of cardiovascular disease is modified by vascular risk groups as measured by the Framingham risk score for coronary heart disease.
Design Prospective cohort study.
Setting Women’s health study, United States.
Participants 27 519 women who were free from cardiovascular disease at baseline with available information on the Framingham risk score and migraine status.
Main outcome measures Time to major cardiovascular disease event (non-fatal myocardial infarction, non-fatal ischaemic stroke, death from ischaemic cardiovascular disease), myocardial infarction, and ischaemic stroke.
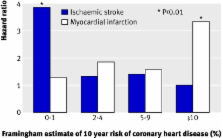
Results At baseline, 3577 (13.0%) women reported active migraine, of whom 1418 (39.6%) reported migraine with aura. During 11.9 years of follow-up, there were 697 cardiovascular disease events. We stratified participants based on 10 year risk of coronary heart disease estimated from the Framingham risk score (≤1%, 2-4%, 5-9%, and ≥10%). Compared with women without migraine, the age adjusted hazard ratios in women with active migraine with aura were 1.93 (95% confidence interval 1.45 to 2.56) for major cardiovascular disease, 1.80 (1.16 to 2.79) for ischaemic stroke, and 1.94 (1.27 to 2.95) for myocardial infarction. When stratified by Framingham risk score, the association between migraine with aura and major cardiovascular disease was strongest in the lowest risk score group. There was a diametric association pattern for ischaemic stroke and myocardial infarction. Compared with women without migraine, the age adjusted hazard ratios in women who reported migraine with aura in the lowest Framingham risk score group were 3.88 (1.87 to 8.08) for ischaemic stroke and 1.29 (0.40 to 4.21) for myocardial infarction. Hazard ratios in women with migraine with aura in the highest Framingham risk score group were 1.00 (0.24 to 4.14) for ischaemic stroke and 3.34 (1.50 to 7.46) for myocardial infarction. Women with migraine without aura were not at increased risk of ischaemic stroke or myocardial infarction in any of the Framingham risk score groups.
Conclusion The association between migraine with aura and cardiovascular disease varies by vascular risk status. Information on history of migraine and vascular risk status might help to identify women at increased risk for specific future cardiovascular disease events.
Trial registration Clinical trials NCT00000479.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women.
- Record: found
- Abstract: found
- Article: not found